A study led by Mayo Clinic researchers has found that nipple-sparing mastectomies (NSM) undertaken to prevent breast cancer are as effective as invasive surgeries for women carrying the BRAC genetic mutation, a known risk factor for developing breast cancer. The findings were presented at the American Society of Breast Cancer Surgeons Annual Meeting (ASBrS 2016) held April 13–17 in Dallas, Texas.
“Nipple-sparing mastectomy is gaining wide acceptance because of its superior cosmetic results, but pockets of the medical community remain skeptical that it is the right choice for the BRCA population,” the study’s lead author, James Jakub, a breast surgeon at the Mayo Clinic in Rochester, Minnesota, said in a recent news release. “This is the largest study of its kind to address the controversy, and to show that nipple-sparing mastectomy is as effective at preventing breast cancer as traditional mastectomy.”
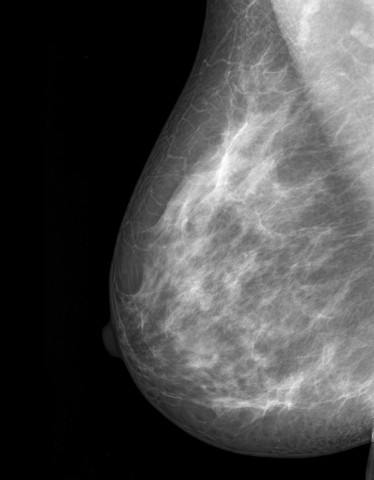
Women opting for preventive mastectomies have been increasingly favoring a nipple-sparing mastectomy (NSM), as this type of surgery leaves the nipple, areola, and breast skin intact, allowing reconstruction of more natural-looking breasts compared to traditional mastectomies. Modern NSM involves complete resection of all gross visible breast tissue, including tissue directly under the nipple.
Researchers examined the incidence of breast cancer in 348 women who were BCRA-positive, and who collectively had undergone 551 preventive NSMs at nine institutions between 1968 and 2013. Specifically, 203 women had a preventive nipple-sparing bilateral mastectomy (both breasts removed), and 145 had NSM in one breast after a cancer in the other.
After a mean follow-up of three to five years, researchers found that none of the women who underwent bilateral NSM developed breast cancer at any site, with no cancer evidence in the retained skin, lymph nodes, or nipples. Seven women died of breast cancer during the follow-up period, but all were women who had a previous or concomitant breast cancer at the time of the procedure.
In 2009, about 8 percent of all mastectomies performed at the Mayo Clinic were NSM, a percentage that rose to about 30 percent in five years, Dr. Jakub said. Still, there is some controversy as to whether NSMs are appropriate for women with BRCA genetic mutations, which increase their breast cancer risk by 50-60 percent by age 70, and up to 80 percent over a lifetime.
“The BRCA population has a genetic mutation in all the cells of their body that predisposes them to breast cancer,” he said. “We know that a majority of breast cancers originate in the breast ducts, so it might seem counterintuitive to leave behind the nipple and the ducts associated with the nipple when you are trying to reduce the risk of this disease.”
According to Dr. Jakub, evidence from published studies has shown that NSM is a safe procedure in women carrying the BCRA genetic mutation, but some doctors want more clinical evidence.
Dr. Jakub believes these findings are further confirmation that NSM is effective in preventing breast cancer in BRCA carriers, and the procedure should be offered to women considering preventive surgery.
“There is no question that this option of nipple-sparing mastectomy can often provide an outstanding cosmetic result and may make it easier for women who are at risk to take this preventive measure,” Dr. Jakub said. “Though the nipple is preserved, it unfortunately will not have stimulation or arousal. Despite that, studies looking at the impact of risk-reducing surgery on quality of life, sexual satisfaction, and intimacy, suggest that being able to preserve aesthetics and body image can improve all of these factors.”