Actress, celebrity, and philanthropist Angelina Jolie’s public revelation in 2013 that she had undergone a prophylactic double-mastectomy, even though she had no breast cancer, gave huge popular awareness to genetic testing for potential cancer susceptibility.
In Jolie’s case, testing revealed that she carries a defective gene, BRCA1, which doctors told her increased her estimated risk of developing breast cancer to 87 percent, and also increased her risk factor for ovarian cancer.
The Jolie example resulted in many more women seeking gene testing for BRCA1 or the related BRCA2 gene, notwithstanding that only some 29 percent of cancers in women originate in the breast, and 5 to 10 percent of women carry high-risk single genes such as BRCA1 and BRCA2.
According to the U.S. National Cancer Institute, BRCA1 and BRCA2 are human genes that produce tumor suppressor proteins that help repair damaged DNA, therefore playing a role in ensuring the stability of the cell’s genetic material. When either of these genes is mutated, or altered, so that its protein product either is not made or does not function correctly, DNA damage may not be repaired properly, resulting in the cells being more likely to develop additional genetic alterations that can lead to cancer.
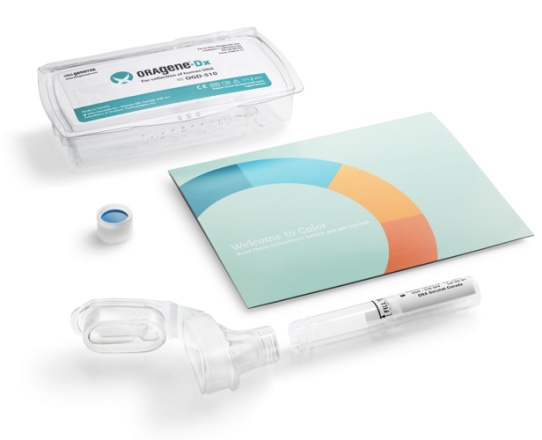
In 2013, the financial cost of having BRCA testing conducted was substantial, typically in the $3,000 to $4,000 range. However, the Silicon  Valley, California-based startup firm Color Genomics Inc. (Color) which says its mission is democratizing access to genetic testing and preventative health information, making it available to women and men in an affordable, high-quality mode, has for the past year been offering its “Color Test” product, described as “a clinical-grade, comprehensive genetic sequencing test,” at the much more more affordable price of $249.
Valley, California-based startup firm Color Genomics Inc. (Color) which says its mission is democratizing access to genetic testing and preventative health information, making it available to women and men in an affordable, high-quality mode, has for the past year been offering its “Color Test” product, described as “a clinical-grade, comprehensive genetic sequencing test,” at the much more more affordable price of $249.
The company says Color Test was originally developed and tested over two years by its team comprised of experts in computer science, distributed systems, machine learning, product design, genetics, and precision medicine, including alumni of Google, Twitter, MIT, the University of California at San Francisco, the University of California at Berkeley, and Stanford University. Co-founders of Color include Elad Gil, Ph.D.; Othman Laraki; Taylor Sittler, M.D.; and Nish Bhat.
“We founded Color because we want to give every person the opportunity to understand their genetic risk of cancer. This important information gives people the opportunity to work with their physician to manage their risk and make key life choices,” explained Color CEO Gil, formerly a cancer researcher at MIT and, more recently, a product and strategy executive at Twitter and Google.
Color Test‘s initial release analyzed 19 major genes known at the time to be responsible for inherited predisposition to breast and ovarian cancer, including BRCA1 and BRCA2. However, Color last month announced broadening the Color Test to cover 30 genes that include many associated with the most common hereditary cancers for both women and men, including breast, colorectal, melanoma, ovarian, pancreatic, prostate, stomach, and uterine cancers, maintaining that genes included on the broader panel can significantly impact an individual’s risk of these cancers. For example, Color cites an APC mutation that can increase risk of colorectal cancer in both women and men to 70 to 100 percent by age 80.
The company notes that all Color’s tests are ordered by a physician — either a customer’s own doctor or one designated by Color — who reviews their information and orders testing on their behalf.
“Building a high-quality, but affordable test required significant investments in software design, big data, bio-informatics, CLIA compliance, laboratory automation, and genetics,” said Laraki, president of Color, at the 2015 product launch. “By marrying multiple emerging disciplines, we have developed something many did not think was possible — a high-quality, yet affordable, genetic test for BRCA1, BRCA2, and 17 other key genes.”
Color also notes that genetic testing for hereditary cancer risk has traditionally been accessible as an insured service according to common reimbursement guidelines only for people with a significant family history of cancer, but that about 50 percent of people who have BRCA1 or BRCA2 mutations do not have a significant family history of the disease, and these individuals have had limited access to genetic testing due to the high cost and a lack of insurance.
 Additionally, Color Genomics offers its Every Woman Program to provide genetic testing to individuals who cannot otherwise afford it. Through the program, Color partners with top cancer centers to ensure genetic testing is available to all women and men — regardless of their financial circumstances.
Additionally, Color Genomics offers its Every Woman Program to provide genetic testing to individuals who cannot otherwise afford it. Through the program, Color partners with top cancer centers to ensure genetic testing is available to all women and men — regardless of their financial circumstances.
Color’s customers also have the option to contribute to the Every Woman program when they purchase a Color Test. Along with Color’s contribution, these sponsorships will provide free testing to women who are unable to afford it.
In February, Color was recognized in the White House Precision Medicine Initiative Fact Sheet, along with the Bill and Melinda Gates Foundation, as an organization that is “Bringing Access to Precision Medicine to All.”
As part of PMI, Color pledged to double the number of underserved individuals who receive the Color Test at no cost through the Every Woman Program in 2016, and also to double the number of Every Woman Program partner cancer centers, which now include:
- University of Washington Medical Center
- UCSF Cancer Genetics and Prevention Program
- University of Pennsylvania Medicines Abramson Cancer Center
- UC San Diego Moore’s Cancer Center
- Morehouse School of Medicine
Last October, Color launched the Color Benefits Program, through which companies can cover part or all of the cost of Color Test testing for their employees, with companies like Visa, Slack, Stripe, and Instacart among the first to make this benefit available to their entire employee population and their families.
However, experts wonder whether speculative genetic testing for potential predisposition to developing cancer is advisable, even at the friendly price of $249 or pro bono.
The U.S. Preventive Services Task Force (USPSTF), in its December 2013 “Final Recommendation Statement – BRCA-related Cancer: Risk Assessment, Genetic Counseling and Genetic Testing,” recommends that primary care providers screen women who have family members with breast, ovarian, tubal, or peritoneal cancer with one of several screening tools designed to identify a family history that may be associated with an increased risk for potentially harmful mutations in breast cancer susceptibility genes (BRCA1 or BRCA2), and says women with positive screening results should receive genetic counseling and, if indicated after counseling, BRCA testing.
However, the USPSTF recommends against routine genetic counseling or BRCA testing for women whose family history is not associated with an increased risk for potentially harmful mutations in the BRCA1 or BRCA2 genes.
The NCI observes that a woman’s lifetime risk of developing breast or ovarian cancer is greatly increased if she inherits a harmful mutation in BRCA1 or BRCA2, noting that about 12 percent of women in the general population will develop breast cancer sometime during their lives. But according to the most recent estimates, 55 to 65 percent of women who inherit a BRCA1 mutation and around 45 percent of women who inherit a BRCA2 mutation will develop breast cancer by age 70.
Regarding ovarian cancer, the NCI estimates that about 1.3 percent of women in the general population will develop ovarian cancer sometime during their lives, but recent research suggests that 39 percent of women who inherit a harmful BRCA1 mutation, and 11 to 17 percent of women who inherit a harmful BRCA2 mutation, will develop ovarian cancer by age 70.
Women who opt to have testing performed and test positive for BRCA1 or BRCA2 mutations will be confronted with the monumental choice of whether to have a preventive mastectomy and oophorectomy (surgical removal of breasts and ovaries) to reduce risk of developing these cancers, and it should be emphasized that a positive test result for one of the mutations does not mean the woman will definitely develop cancer, so it’s a difficult decision to make.

 The Cleveland Clinic’s Charis Eng, M.D., Ph.D., also chairwoman of the Genomic Medicine Institute and founding director of its Center for Personalized Genetic Healthcare, advises that if you’re concerned because of your family history or other red flags for cancer, “Don’t hesitate: Ask to visit a genetic counselor. They can assess your history and test you for a mutation if needed. It’s a crucial step in knowing whether you are at risk — and what you can do to reduce that risk.
The Cleveland Clinic’s Charis Eng, M.D., Ph.D., also chairwoman of the Genomic Medicine Institute and founding director of its Center for Personalized Genetic Healthcare, advises that if you’re concerned because of your family history or other red flags for cancer, “Don’t hesitate: Ask to visit a genetic counselor. They can assess your history and test you for a mutation if needed. It’s a crucial step in knowing whether you are at risk — and what you can do to reduce that risk.
“Having both of your breasts removed does not take your chance of breast cancer down to zero,” Eng said. “But it does take the risk down to the single digits, a big difference from 80 percent. Removing the ovaries offers similar results. Women who choose these procedures should still be monitored for life, but they also may spend less time fretting over the future.”
“These decisions are never easy,” Eng added. “They’re also highly personal. “Many women will opt for careful monitoring rather than surgery. It comes down to you and your doctors considering all the available information and — just as Ms. Jolie did — making the right choice for you.”
 The Cleveland Clinic offers a free Breast Cancer Treatment Guide that may be helpful in making an informed decision.
The Cleveland Clinic offers a free Breast Cancer Treatment Guide that may be helpful in making an informed decision.
The NCI also says genetic counseling is generally recommended before and after any genetic test for an inherited cancer syndrome, and this should be performed by a healthcare professional who is experienced in cancer genetics.
Persons considering having genetic testing done may also find the NCI’s fact sheet on genetic testing for cancer risk helpful.