Women with breast cancer who undergo breast-conserving surgery and a type of internal radiation therapy known as brachytherapy are more likely to require additional breast biopsies during their follow-up care, a nationwide study shows.
However, the overall rates of biopsy were relatively low, and most patients will not need additional cancer treatment.
The study, titled “Incidence and Outcome of Breast Biopsy Procedures During Follow-up After Treatment for Breast Cancer,” was published in the journal JAMA Surgery.
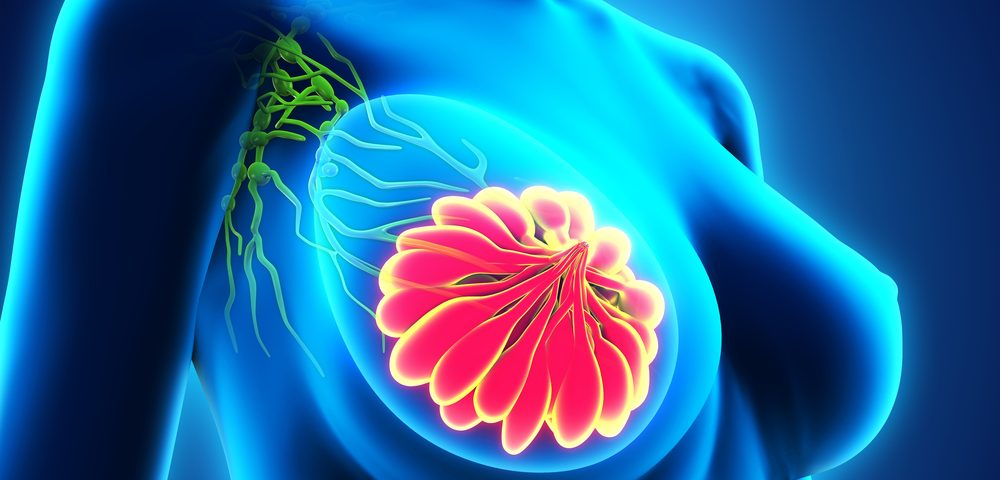
The two main surgical options for the treatment of breast cancer are breast-conserving surgery (BCS) — the cancer is removed while leaving as much normal breast as possible — with radiation, or mastectomy. Previous studies have shown that these procedures have equivalent long-term survival rates.
However, many patients choose to undergo mastectomy due to the fear of repeated breast biopsies during follow-up, and the possibility of another breast cancer diagnosis. Currently, data on the biopsy rates after BCS or mastectomy remains unclear.
Using two national databases that included younger and older women with insurance, researchers at The University of Texas MD Anderson Cancer Center investigated how often follow-up biopsies were performed in 121,879 breast cancer patients.
The retrospective study included 41,510 women younger than 65 years and 80,369 women age 66 years and over who were diagnosed with invasive breast cancer (stages I – III) between January 1, 2000 and December 31, 2011. The data on the younger women came from MarketScan (the national database of patients with private insurance) and the data on the older women came from the National Cancer Institute’s SEER-Medicare Database (SEER is an acronym for Surveillance, Epidemiology, and End Results).
Mean patient age was 52.8 years for the MarketScan group of patients, and 76.3 years for the SEER-Medicare group. While BCS was performed in around 60 percent and mastectomy in about 40 percent of the younger patient group, the figures were reversed in the older group of patients.
The five- and 10-year rates of breast biopsy were 14.7 percent and 23.4 percent, respectively, in the younger group and 11.8 percent and 14.9 percent, respectively, in the older group.
Among patients treated with unilateral mastectomy, the five-year incidence of breast biopsy was 10.4 percent in the younger group and 7.8 percent in older group. Biopsy rates were higher in all women treated with BCS (alone, with whole-breast irradiation, or with brachytherapy), ranging from 9.4 to 25 percent.
Patients who received BCS and whole-breast irradiation had an incidence of biopsy of 16.7 percent in the younger group and 15.1 percent in the older group. In both groups, BCS and brachytherapy showed the higher biopsy rate – 24 percent in the younger group and 25 percent in the older group.
Younger age was associated with increased risk of breast biopsy, and older women who received adjuvant chemotherapy were also more likely to undergo breast biopsies. Endocrine therapy was found to have a protective effect against relapse, being associated with a lower risk of biopsy.
Among patients who had a breast biopsy after initial therapy, 29.8 percent of the younger group and 23.2 percent of the older group of women underwent additional cancer treatment.
“The important message is that the rate of biopsy for patients is relatively low and the overwhelming majority of the biopsy results will be benign and not require further treatment,” Henry Kuerer, MD and the study’s senior author, said in a press release.
The team also noted that the study had some limitations. They only analyzed data from three months after biopsy to determine subsequent treatment, which may not be representative, and the 10-year follow-up period may be short for many women with breast cancer.