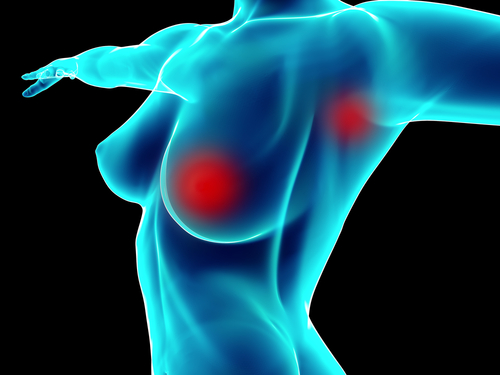
Researchers from the Stanford University School of Medicine and the Cancer Prevention Institute of California have discovered that breast cancer patients treated with lumpectomy followed by radiation therapy have the same survival rate as patients who had bilateral mastectomy (removal of both breasts).
Researchers from the Stanford University School of Medicine and the Cancer Prevention Institute of California have discovered that breast cancer patients treated with lumpectomy followed by radiation therapy have the same survival rate as patients who had bilateral mastectomy (removal of both breasts).
This surgical technique is increasingly used to treat unilateral breast cancer, giving rise to medical and psychosocial complications. As such, the need for a better understanding of its use and outcomes is essential towards optimization of cancer care.
In a study entitled “Use of and Mortality After Bilateral Mastectomy Compared With Other Surgical Treatments for Breast Cancer in California, 1998-2011” and published in the Journal of the American Medical Association, the researchers compared the use of and mortality after bilateral mastectomy, lumpectomy (the selective removal of cancerous tissue within the breast) plus radiation, and unilateral mastectomy (the removal of the affected breast).
“Given the recent attention around bilateral mastectomies, we wanted to know whether there are particular types of patients likely to receive a bilateral mastectomy. And, secondly, are there relative differences in mortality among the three procedures? We were able to address these questions using data from the California Cancer Registry, which covers nearly all women diagnosed with breast cancer in the state. The registry is enhanced with information on factors that may influence a treatment decision, including their socioeconomic status, health insurance and where they received their care”, senior author Scarlett Gomez, PhD, research scientist at CPIC said in a Stanford University press release.
[adrotate group=”3″]
The team designed a comprehensive cohort study within the population-based California Cancer Registry, analyzing 189,734 women who had been diagnosed with stages 0-III unilateral breast cancer in California from 1998 through 2011. They observed that in 2011, up to 12% of all newly diagnosed breast cancer patients chose to preform a bilateral mastectomy, even though they were uncertain if this approach was better than the remaining alternatives.
“We can now say that the average breast cancer patient who has bilateral mastectomy will have no better survival than the average patient who has lumpectomy plus radiation. Furthermore, a mastectomy is a major procedure that can require significant recovery time and may entail breast reconstruction, whereas a lumpectomy is much less invasive with a shorter recovery period,” lead author Allison Kurian, MD, an assistant professor of medicine and of health research and policy at Stanford also added in the press release.
The results showed that within the total population studied, 55% received a lumpectomy with follow-up radiation, 38.8% had a unilateral mastectomy, and 6.2 % received a bilateral mastectomy, with the proportion of women receiving unilateral mastectomies declining throughout the study period and the proportion of women receiving bilateral mastectomies increasing.
Furthermore, women from racial and ethnic minorities, along with women of lower socioeconomic status, had higher chances of receiving a unilateral mastectomy than women from middle- or upper-class, younger than 50, or non-Hispanic whites.
Importantly, women who received a bilateral mastectomy or a lumpectomy plus radiation had approximately the same long-term survival rates.
The registry database used to design this study provides important information about almost every cancer case in the state, including stage of the disease, surgical outcome chosen both by the patient and physician, survival outcome and racial or ethnic background information.
“The registry allows us to do a population-based study to gain a real-world picture of cancer cases in California. We can ask and answer questions that couldn’t be answered in a randomized clinical trial”, Dr. Kurian explained.
Even though women undergoing bilateral mastectomy did not show improved survival rates, the study revealed that there are growing numbers of women deciding to perform the complex surgery that requires a long recovery period and can result in reconstructive surgery.
Nonetheless, the authors noted that if a woman is diagnosed with a BRCA1, BRCA2 or other gene mutation that significantly increases the chances of developing breast cancer, or has a family history of breast cancer, bilateral mastectomy could be an appropriate option.
“We’re hopeful that this study will open a dialogue between a patient and her physician to discuss these kinds of questions. It’s an important piece of evidence that can guide their decision-making process,” concluded Dr. Gomez in the press release.
The results from this study can lead to a better evaluation of the risk-benefit ratio of bilateral mastectomy, allowing a better understanding of breast surgery use and enhancing the quality of cancer care.