Researchers have developed a technique that showed potential to identify estrogen receptor (ER)-positive breast cancers much faster and easier than current methods, potentially speeding a patient’s diagnosis and advancing the possibility of more personalized treatment.
The study detailing their work, “Correlating nuclear morphometric patterns with estrogen receptor status in breast cancer pathologic specimens,” was published in the journal npj Breast Cancer.
Treatment decisions and patient management in breast cancer depends greatly on the presence of specific markers – cancer cells with receptors for estrogen and other hormones – as these markers are associated with different responses to current therapies.
ER-positive breast cancers account for more than 70 percent of all such cancers, and these patients are often treated with one of two classes of therapies after surgery.
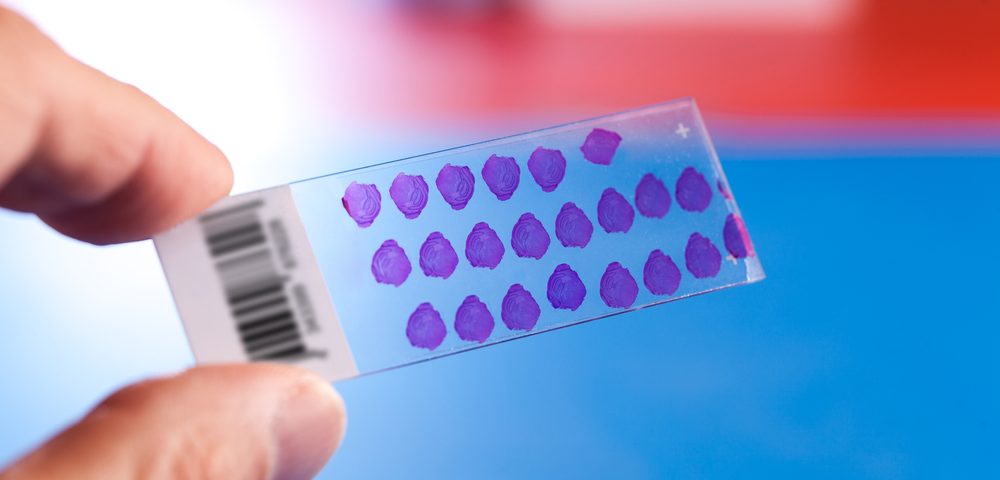
In the U.S., the standard procedure to characterize breast tumors uses immunohistochemistry, a method in which biopsies slides are analyzed under a microscope for the presence of specific markers.
However, this process is expensive, slow – taking weeks to provide results – and somewhat inconsistent, as different laboratories may reach different results.
Increasingly, data point to a link between changes in the morphology of the cell, or its internal components, and the presence of specific markers.
Researchers led by a team at the University of Southern California developed a technique based on machine learning that can distinguish ER-positive from ER-negative breast cancer through the analysis of the morphology of the cells’ nucleus – the specialized structure that contains a person’s genetic information, and controls and regulates the cell’s activities.
They used publicly available tissue images (labeled with only a standard procedure) of 113 breast cancer patients and their corresponding ER status (determined by immunohistochemistry).
Fifty-seven of these images were used to train a computer to associate specific nuclear features, such as shape and orientation, to ER-positive or ER-negative status.
When the team tested the machine on the tissue images of the remaining 56 patients, it could predict with accuracy the ER-status of the samples based on those nuclear features.
While the standard approach may take weeks to identify a marker after diagnosis, “with machine learning technology, we can tell you the same day, so there’s less delay, less stress and potentially better outcomes,” Daniel Ruderman, a study author, said in a press release.
“It’s going to enable us to identify the right drug and dose more quickly. It’s a big step toward personalized medicine,” Ruderman added.
Additional analysis revealed that ER-negative tumors seemed to be associated with larger, more variable nuclei (in several features) than ER-positive tumors. The team believes its approach also has the potential to identify new cellular features and patterns associated with specific types of breast cancer and treatment response.
While the results are promising, further validation is needed before the technique might be applied in the clinical setting, and the researchers expect that tests involving larger groups of patients will also improve the machine’s predictive accuracy.