During the American Society for Radiation Oncology’s (ASTRO’s) 56th Annual Meeting at the Moscone Center in San Francisco, September 14-17, 2014, a study entitled “The Impact of Radiation Therapy on Lymphedema Risk and the Agreement Between Subjective and Objective Lymphedema Measures: NSABP B-32 Secondary Data Analysis,” was presented, showing that radiation therapy (RT) does not increase the incidence of lymphedema in patients with node-negative breast cancer. This study was conducted by Susan McCloskey, MD, MSHS, assistant professor of radiation oncology at The David Geffen School of Medicine at University of California, Los Angeles.
During the American Society for Radiation Oncology’s (ASTRO’s) 56th Annual Meeting at the Moscone Center in San Francisco, September 14-17, 2014, a study entitled “The Impact of Radiation Therapy on Lymphedema Risk and the Agreement Between Subjective and Objective Lymphedema Measures: NSABP B-32 Secondary Data Analysis,” was presented, showing that radiation therapy (RT) does not increase the incidence of lymphedema in patients with node-negative breast cancer. This study was conducted by Susan McCloskey, MD, MSHS, assistant professor of radiation oncology at The David Geffen School of Medicine at University of California, Los Angeles.
ASTRO’s 56th Annual Meeting is the nation’s leading scientific meeting in radiation oncology and is expected to attract more than 11,000 attendees from a wide group of disciplines, from medical physicists to practice administrators, industry representatives, and other health care professionals from around the world. This year’s annual meeting’s theme is “Targeting Cancer: Technology and Biology.” The Presidential Symposium, “Local-regional Management of Breast Cancer: A Changing Paradigm,” is being led by ASTRO President Bruce G. Haffty, MD, FASTRO, a radiation oncologist specializing in breast cancer, and Jay R. Harris, MD, FASTRO, and Thomas A. Buchholz, MD, FASTRO. During the ASTRO’s four-day scientific meeting, three keynote speakers will address a range of topics including oncologic imaging, biology and targeting in oncology, and human error and safety concerns: Hedvig Hricak, MD, PhD, Chair of the Department of Radiology and the Carroll and Milton Petrie Chair at Memorial Sloan Kettering Cancer Center; Frank McCormick, PhD, FRS, DSc (hon), Professor Emeritus and the David A. Wood Distinguished Professor of Tumor Biology and Cancer Research of the University of California at San Francisco Helen Diller Family Comprehensive Cancer Center; and Sidney Dekker, PhD, MA, MSc, Professor and Director of the Safety.
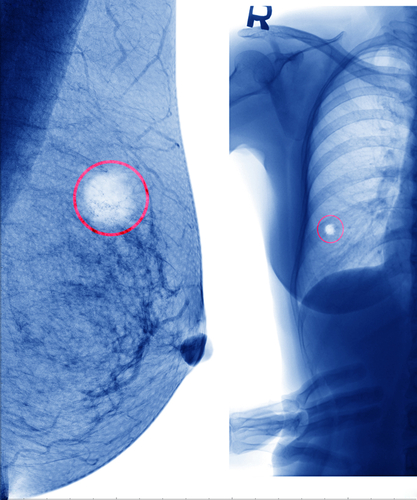
The novel study, NSABP B-32, was a randomized trial of sentinel node biopsy (SNB) versus SNB + axillary lymph node dissection (ALND) in 5,611 women with clinically node-negative breast cancer. This study was designed primarily to determine if SNB was as effective as ALND with fewer side effects, i.e. the impact of type of axillary surgery specifically on lymphedema risk, but it also provided the opportunity to evaluate the impact of radiation therapy (RT) on lymphedema risk. In SNB, only a few lymph nodes are removed and examined for signs of cancer, while ALND involves removing most lymph nodes under the arm on the same side as the breast tumor and examining the nodes for signs of cancer spread. Lymphedema is the swelling of the arm due to a build-up of lymph fluid usually caused by the removal of or damage to lymph nodes and is a consequence of locoregional breast cancer therapies.Though it is difficult to assess if lymphedema formation is due to surgery or radiation therapy (RT).
[adrotate group=”3″]
This study consisted of measuring lymphedema in patients with node-negative breast cancer by standardized arm measurements done by clinicians, called objective lymphedema, and defined as relative arm volume difference (RAVD) > 10 percent, as well as through questionnaires completed by patients, called subjective lymphedem, and defined by ipsilateral (occurring in the same arm) swelling that was “somewhat,” “quite” or “very” bothersome, before RT and every 6 months during the 3-year follow-up period.
This clinical trial included 3,916 women, 1,936 and 1,980 were randomly assigned, respectively, to SNB+ALND and SNB, and 82.2 percent (3,220) received RT and 17.2 percent (674) did not undergo RT. For 0.6 percent (22) of the patients, the status was unknown. The results from the first study showed that SNB+ALND treatment was associated with significantly greater risk of lymphedema then the SNB treatment alone. After a secondary analysis, the researchers found that there were no significant differences in standardized measurements of the arm or in patient reports of bothersome arm swelling during three years of follow-up between the groups of women that received RT and not received RT. Interestingly, it was observed that subjective lymphedema, defined as bothersome to patients, was less frequent (8% ALND and 3.5% SNB at 36 months) and had a poor agreement with objectively measured RAVD > 10%. Therefore, the researchers are performing other analyses of objective data to assess methods of quantification that may better correlate with subjective assessments.
“These results provide much needed reassurance to breast cancer patients regarding the impact of radiation therapy on lymphedema risk,” said Susan McCloskey. “The study findings argue convincingly that radiation therapy to the Level 1 axilla, considered unavoidable “collateral damage” when radiating the whole breast, does not contribute to lymphedema risk beyond surgery. Several recent analyses have suggested that mastectomy rates are on the rise in the United States, and some have suggested that a desire to avoid radiation and its associated toxicities is a contributing factor. This analysis suggests that lymphedema concerns should not be an impediment to women choosing breast conservation and radiation therapy,” added McCloskey.