 A group of researchers from the Vanderbilt University School of Medicine, Nashville, Tennessee, recently published a study entitled, “Efferocytosis produces a prometastatic landscape during postpartum mammary gland involution” in the Journal of Clinical Investigation, where they demonstrate that during the first 5 years after the birth of a child, women are at an increased risk of developing metastatic breast cancer.
A group of researchers from the Vanderbilt University School of Medicine, Nashville, Tennessee, recently published a study entitled, “Efferocytosis produces a prometastatic landscape during postpartum mammary gland involution” in the Journal of Clinical Investigation, where they demonstrate that during the first 5 years after the birth of a child, women are at an increased risk of developing metastatic breast cancer.
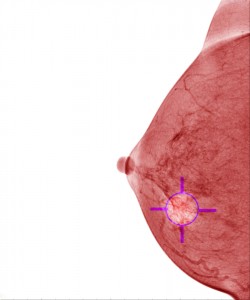
In the first postpartum years, women who are diagnosed with breast cancer have a higher probability of having a metastatic malignancy, which correlates with much poorer outcomes and low survival rates.
However, the molecular mechanisms underlying the malignant severity associated with postpartum breast cancers (ppBCs) are still not understood, but some available data correlate it with stromal wound-healing events during postpartum involution, a biological process where milk-producing mammary epithelial cells (MECs) begin to die through apoptosis.
The research team used mice models of spontaneous and allografted mammary tumors and observed that postpartum involution was linked to mammary tumor metastasis and increased cell death both in MECs and in the tumor epithelium.
Furthermore, they found that receptor tyrosine kinase MerTK–dependent phagocytosis was responsible for clearing dying tumor cells, by inducing cytokines such as IL-4, IL-10, IL-13, and TGF-β.
[adrotate group=”3″]
Animals that were either genetically deficient for MerTK or were treated with MerTK inhibitors, could not efficiently clear tumor cells in postpartum tumors, had decreased M2-like macrophages, TGF- β expression and a reduction of postpartum tumor metastasis.
These results suggest that the increased tumor cell death observed during postpartum involution is responsible for the initiation of efferocytosis, or tumor cell clearance via phagocytic macrophages, which express the MerTK receptor on the surface of their cell membranes. This in turn induces a stromal wound-healing process that can enhance tumor malignancy, allowing breast cancer cells to gain metastatic potential.
This knowledge can help pave the way for future research towards improved strategies that could allow prevention and treatment of postpartum breast cancers.

