 Tumor-infiltrating lymphocytes (TILs) can be used to treat cancer and has prognostic/predictive indicators.
Tumor-infiltrating lymphocytes (TILs) can be used to treat cancer and has prognostic/predictive indicators.
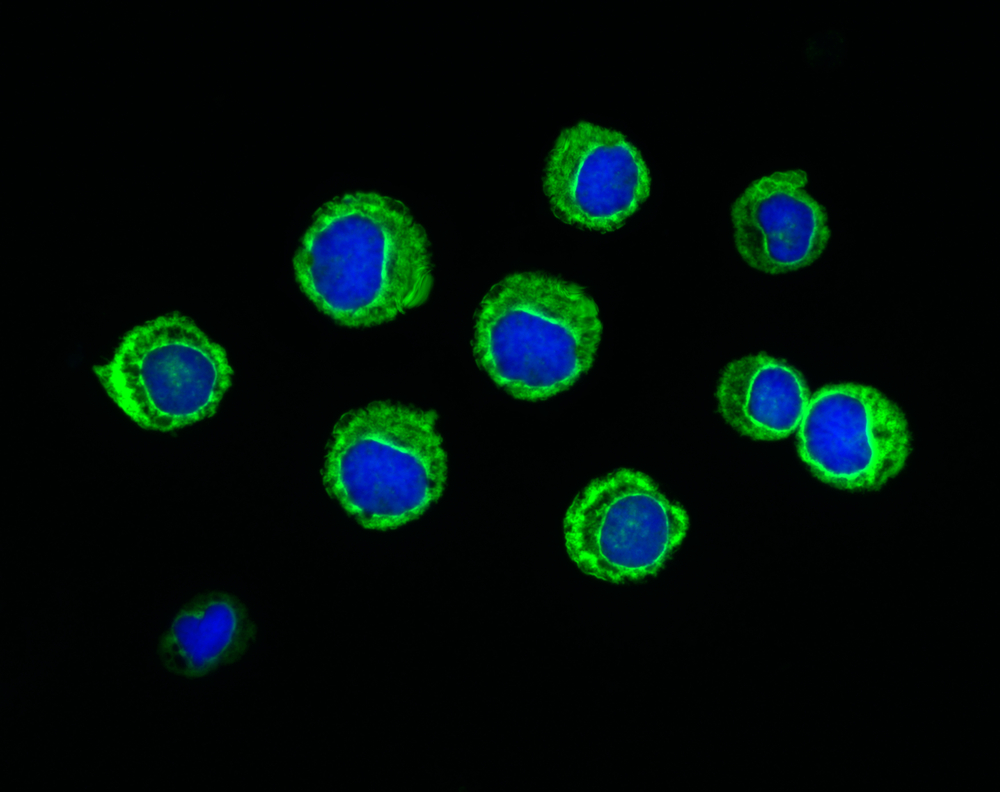
Solid tumors are made of several components such as malignant cells and endothelial cells, as well as structure and immune cells. Cancer cells have the ability to shape the microenvironment around them to satisfy their metabolic and immunological needs. To fight that ability, TILs are recruited into the tumor as a way to control its growth. Importantly, patients respond to a cancer treatment according to the amount of TILs in their tumor microenvironment. As such, TILs can be associated with prognosis and can be manipulated to be used as treatment against the patient’s own cancer.
Many studies suggest that marked infiltration of specific immune cell populations can be a good or poor prognostic to overcome cancer. Cancer cells express antigens that differentiate them from healthy cells. However, tumour-associated antigens are normal proteins expressed in higher amounts, allowing them to be tolerated by the immune system.
Immune selection pressure on genetically unstable tumor cells leads to selection of tumour cells that are no longer recognized by adaptive immunity (for instance due to defects in antigen processing or due to antigen loss). Hence, they induce tolerance within their microenvironment and their growth can no longer be stopped by immunity response. These cells can re-appear and cause metastatic disease.
[adrotate group=”3″]
Studies suggest that breast cancer is immunogenic. The prognostic implications of TILs in triple-negative breast cancer (TNBC) and associations with trastuzumab benefit in HER2-overexpressing disease were presented at the European Society for Medical Oncology (ESMO) 2014 meeting. A positive association between the amount of TILs present at diagnosis and prognosis in TNBC was concluded, however the same was not verified for luminal or HER2-positive subtypes. Further, an interaction between higher levels of TILs and an increased benefit from trastuzumab was found: an 18 percent reduction in the relative risk of recurrence for each 10 percent increase in lymphocyte infiltrate.
The prognostic capability of TILs in TNBC has been demonstrated even though it can result from a number of different factors. Genetic instability and heterogeneity of tumours leads to a selection of variants that can stimulate a host immune response against the tumour. Better prognosis in patients with TNBC and higher TILs is the outcome of an immunoediting process induced by chemotherapy. Tumor cells that are dying during chemotherapy cause an immunological reaction against the tumor cells, stimulating the immune system to recognize and destroy malignant cells.
Importantly, the immune system has the ability of remembering what it targets, providing a durable response against tumours.