 Mayo Clinic researchers have assessed the diagnostic performance of supplemental screening women with dense breasts using molecular breast imaging (MBI) to allow for radiation dose reduction.
Mayo Clinic researchers have assessed the diagnostic performance of supplemental screening women with dense breasts using molecular breast imaging (MBI) to allow for radiation dose reduction.
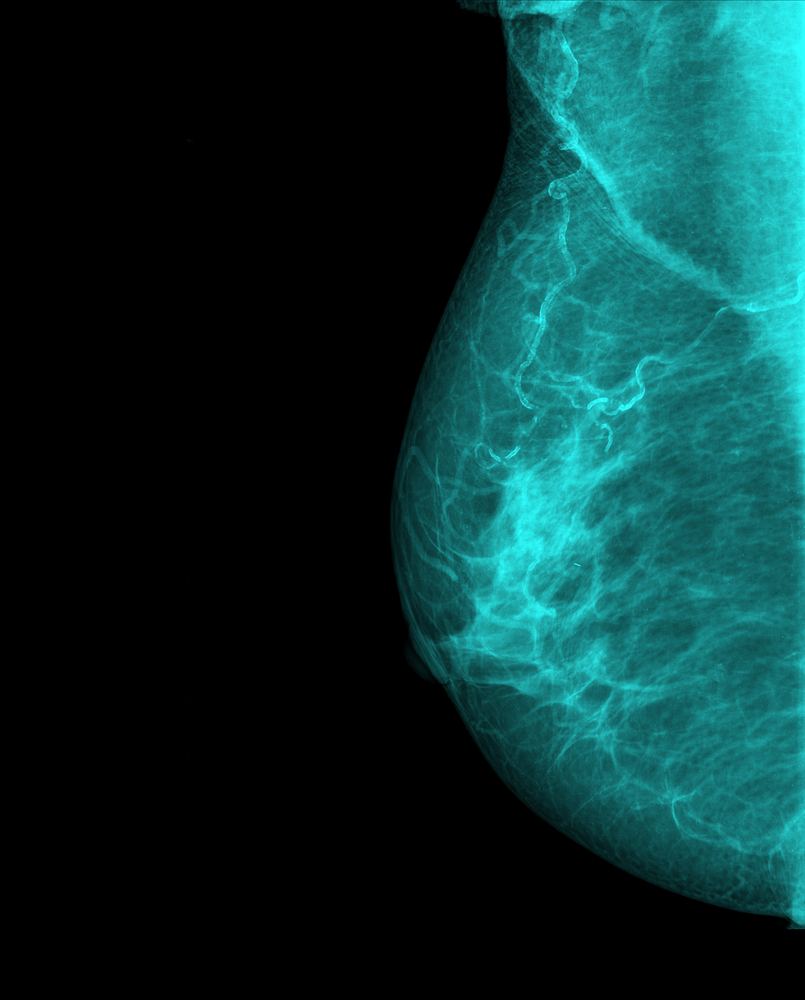
The efficacy of digital screening mammography is significantly lower in women who have dense breasts (accounting for approximately 50% of all screening-aged population).
Within 19 states across the country, it is already mandatory that women who undergo mammography be informed that they may benefit from supplemental screening if they have mammographically dense breasts. However, a consensus has not yet been reached about the best imaging technique for additional screening, along with the balance of its benefits and harms.
In this study, titled “Molecular Breast Imaging at Reduced Radiation Dose for Supplemental Screening in Mammographically Dense Breasts”, published in the American Journal of Roentgenology, researchers screened a total of 1,651 asymptomatic women with mammographically dense breasts using two-view digital screening mammography and two-view MBI (Discovery NM 750b, GE Healthcare, or LumaGem, Gamma Medica), which were independently analyzed by different radiologists blinded to the other imaging test. Furthermore, breast biopsies were made after completion of both tests.
Of the total women who enrolled in the study, 1,585 met the eligibility criteria. These women’s cancer status was confirmed using pathology findings (2.5%), negative imaging findings (96.1%), clinical examination (0.1%), and patient interview (1.3%).
[adrotate group=”3″]
The results demonstrated that adding MBI screening enhanced cancer detection rate when compared to mammography alone. Furthermore, adjunct MBI increased sensitivity from 23.8% (mammography alone) to 90.5% (combination). Researchers further noticed that MBI was more sensitive for invasive cancer detection than mammography. “Approximately 80% of cancers seen only on MBI were invasive, suggesting that MBI is not selectively detecting clinically unimportant cancers. Eighty-two percent of the invasive cancers seen only on MBI were node negative, suggesting that MBI contributes to early detection of clinically important cancers”, the authors write in their study. “MBI also detected larger and node-positive invasive cancers that were mammographically occult, suggesting a role for MBI in identifying cancers masked on repeated mammographic screenings by dense breast parenchyma”, they add.
The team concludes that MBI used in addition to mammography in women who have dense breasts could “exploit what mammography finds and find what mammography misses, preserving the cancer detection rate found in this study without the additional costs and false-positive findings associated with supplemental screening”.