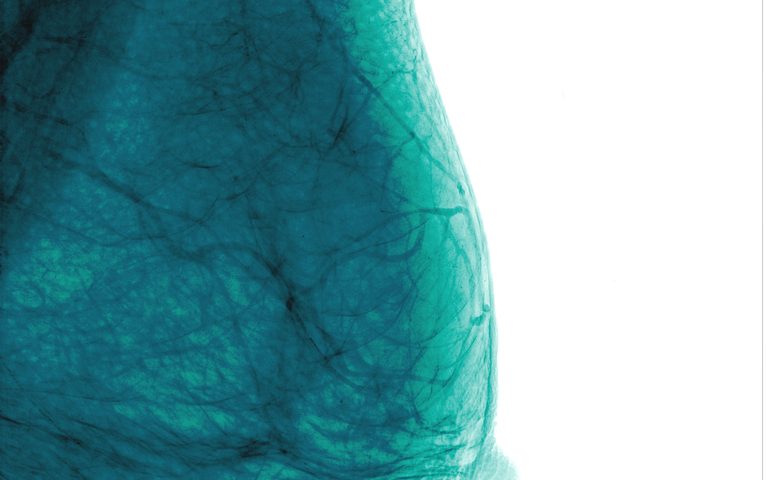
Researchers from Finland recently discovered that women with a very low breast density, detected by mammography scans, often have a worse prognosis if they develop breast cancer. Such a link is even stronger in tumors containing high levels of hyaluronan, a common component of soft connective tissue, demonstrating that prognostic tools in breast cancer can be optimized.
Breast density has been most widely discussed as a risk factor for breast cancer, where earlier studies have noted that women with high density get cancer about four to six times as often than other women.
So far, however, no studies have examined if breast density affects disease aspects in women who already have cancer, and clinicians in the field agree that more accurate markers of disease progression would allow a more personalized treatment approach.
A doctoral thesis by Amro Masarwah at the University of Eastern Finland and Kuopio University Hospital in Finland examined 278 women with breast cancer, following them over time.
The thesis, titled “Mammographic Breast Density, Tumour Characteristics and the Expression of Hyaluronan as Prognostic Surrogate Markers for Breast Cancer,” found that very low breast density was linked to worse prognosis and lower survival rates, showing that there are likely different mechanisms at work during tumor development and later progression and growth.
Exploring how the presence of hyaluronan affected the relationship, scientists found that low breast density often went hand in hand with high levels of hyaluronan. Combining breast density and hyaluronan levels in an analysis showed that the two factors in concert resulted in an even worse prognosis and a lower likelihood that a patient survives.
There are currently a number of other factors used to assess prognosis in breast cancer patients, and the study found that in this group, levels of the breast cancer factor HER2 (human epidermal growth factor receptor 2) could also be linked to prognosis, with higher levels present in women with a worse disease course.
The Nottingham Prognostic Index, a tool used to evaluate prognosis in breast cancer patients who have undergone surgery, does not take into account either breast density or HER2 levels. Adding these factors to the index, Masarwah developed an improved tool, called the Kuopio-Nottingham Prognostic Index, which could better predict prognosis in women with breast cancer.
Masarwah hopes the findings will benefit doctors and patients in the near future. “Since measuring density is becoming more common, physicians’ expertise with density will increase and this will open up doors for mammographic breast density to be used in patient outcome prediction,” he said in a press release.