Routine management of patients diagnosed with ductal carcinoma in situ (DCIS), the most common type of non-invasive breast cancer, typically includes a needle biopsy to determine if the tumor is invasive or non-invasive and to test for estrogen receptors (ER) and progesterone receptors (PR). But according to a new study conducted by pathologists from Johns Hopkins University School of Medicine in Baltimore, Md., the ER/PR tests are unnecessary and wasteful.
The study, “Reflex Estrogen Receptor (ER) and Progesterone Receptor (PR) Analysis of Ductal Carcinoma In Situ (DCIS) in Breast Needle Core Biopsy Specimens: An Unnecessary Exercise That Costs the United States $35 Million/y,” published in The American Journal of Surgical Pathology, suggests that ending the practice could save approximately $35 million per year in the United States alone.
In DCIS patients particularly, patients with receptor-positive DCIS respond well to relatively medications, such as tamoxifen, that help prevent DCIS from recurring after surgery. But according to the researchers, five factors suggest that testing needle core biopsies for hormone receptors is basically unnecessary.
First, regardless of the results of the core biopsy for estrogen receptors (ER) or progesterone receptors (PR), standard of care for DCIS patients in the U.S. is the next step (second factor) — surgical removal of the suspected breast tissue, either by lumpectomy or mastectomy. In some cases, patients who were first diagnosed with DCIS through the core needle biopsy, are actually found to have an accompanying invasive breast cancer. In these cases, the same test needs to be performed again to assess whether the invasive tissue is positive for the hormone receptors — meaning that the initial test was useless.
In the remaining 80 percent of cases in which the surgical excision contains DCIS alone, if the first core biopsy was negative, (third factor) the physician usually recommends that the surgically removed tissue is tested again because hormone expression can be heterogeneous within the same tumor, and the small biopsy could have missed a positive area.
The fourth reason is that many patients with receptor-positive DCIS decline hormone therapy after surgical excision anyway. Finally, although hormone-blocking therapies for receptor-positive DCIS can reduce the risk of tumor recurrence, the therapy does not affect patient’s survival.
Researchers reviewed the pathology and medical records of 58 patients who were diagnosed with DCIS based on the core needle biopsies.
“Two-thirds of our DCIS study patients did not receive hormone therapy even after excision confirmed their hormone-receptor positive DCIS status,” said Dr. Pedram Argani, professor of pathology and oncology at the Johns Hopkins University School of Medicine, and senior author of the study, in a press release. “So analyzing their needle biopsies or surgical excisions for receptors would have clearly been unnecessary for them.”
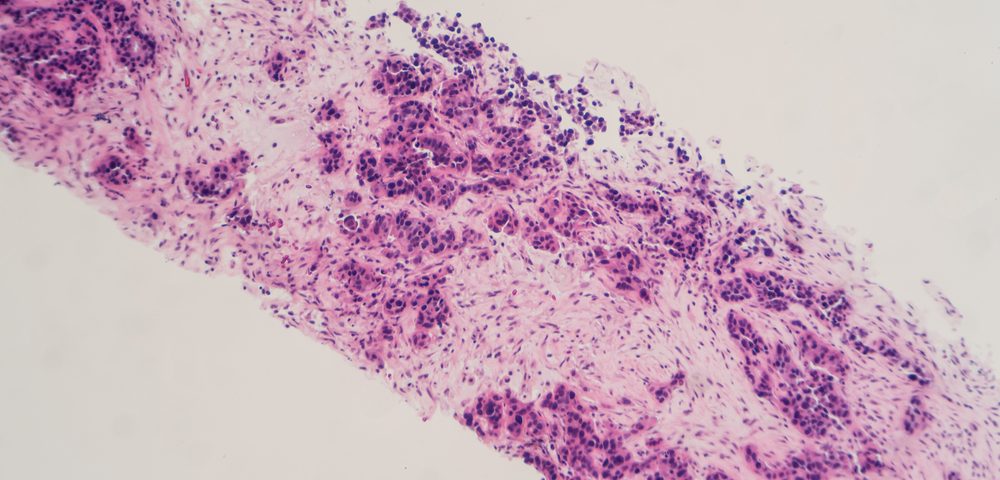
The team notes that early receptor analysis costs about $140.00 per patient. This includes the staining of the biopsy with antibodies against the receptors, with a technique called immunohistochemistry, and the pathologist’s time to study it.
“If you apply our local results nationally, these unnecessary initial hormone receptor tests currently come with an annual price tag of around $35 million,” said Argani. “Our results indicate that’s an expense without any justification. If these tests were routinely eliminated, the savings would be substantial.”