High breast density is strongly associated with a risk of breast cancer, because dense breasts can mask a cancer from being detected during a mammography screening.
An estimated 40 percent of women have dense breast tissue, and standard mammography is effective only about 48 percent of the time in detecting lesions in dense breasts (as compared to 98 percent in fatty breasts). This means that every second or third cancer may be missed in women with dense breasts, according to Are You Dense Advocacy, an organization working to increase awareness of the problems and in finding ways of addressing it.

 A team of researchers at the University of Malaya, led by a professor of medical physics at the Department of Biomedical Imaging, Ng Kwan Hoong, published two papers on the subject of breast density and its association with breast cancer, noting that breast cancer risk because of high breast density is two times greater than other factors (with the exception of a family history of the disease in women ages 40-49). But whether breast density is an independent risk factor remains a matter of debate.
A team of researchers at the University of Malaya, led by a professor of medical physics at the Department of Biomedical Imaging, Ng Kwan Hoong, published two papers on the subject of breast density and its association with breast cancer, noting that breast cancer risk because of high breast density is two times greater than other factors (with the exception of a family history of the disease in women ages 40-49). But whether breast density is an independent risk factor remains a matter of debate.
In recognition of his research and efforts, Hoong was recipient of the 2016 International Day of Medical Physics (IDMP) Award presented at the 22nd IDMP, Dec. 9-12, in Bangkok, Thailand. The award recognizes excellence in medical physics, both in terms of promoting the discipline to a larger audience and in terms of contributions made by medical physicists for patient care.
The first of the two papers, “Standardisation of clinical breast-density measurement,” was published in 2012 in The Lancet Oncology, and the second, “Vision 20/20: Mammographic Breast Density and its Clinical Applications,” appeared in 2015 in the journal Medical Physics. The 2012 paper highlights the need for standardized protocol in breast density measurement, while the 2015 article provides a comprehensive review of breast density measurement over the past 40 years, along with current and future applications in earlier detection of breast cancer.

The challenge in assessing breast density, the Lancet paper notes, lies in there being no standard common understanding of breast density and in several different methods being used to measure it, including the Breast Imaging Reporting and Data System (BI-RADS), Boyd’s six category classification, and Tabar. Researchers caution that the term ‘visually assessed’ is an inherent cause for concern, since such assessments are subjective and dependent on the reporting radiologist’s skill and experience. While an experienced radiologist would be aware of variables that could affect readings, such as the X-ray exposure used, adequacy of compression, and positioning of the breast, in a less skilled radiologist’s hands, results could vary considerably.
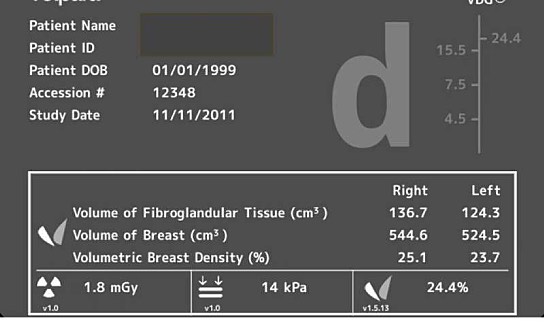
There is good news as well. Commercial software to measure volume density, that can be used to complement routine mammography, is becoming available; these include the R2 Quantra (Hologic), Volpara (Matakina), Spectral (Philips) and M-Vu (VuComp) programs. The Ng team notes that the software’s robustness and acceptance by the international community have not been established, but merit investigation.
The team also advocates the development of an international standard protocol for assessing breast density, maintaining that because breast density information is relevant in clinical choices for screening, diagnosis, intervention, and management of breast cancer, then standardized, reliable, and reproducible breast-density measurement techniques are needed to facilitate more accurate analysis and risk prediction.
They project that, in the long term, with development of a standardized screening protocol, tracking global and regional breast density changes over time will be possible, allowing for earlier detection of breast cancers and their treatment.

