Applying radiation therapy to lymph nodes behind the breast bone and above the collar bone can improve outcomes for earlier-stage breast cancer patients, with limited side effects, Phase 3 long-term data show.
Data found that 15 years after such treatment, 73.2 percent of patients given this more extensive radiation were alive, compared to 70.8 percent of those who underwent standard of care.
The research, “Fifteen-year results of the randomised EORTC trial 22922/10925 investigating internal mammary and medial supraclavicular (IM-MS) lymph node irradiation in stage I-III breast cancer,” was presented at the ongoing 2018 American Society of Clinical Oncology (ASCO) Annual Meeting, in Chicago.
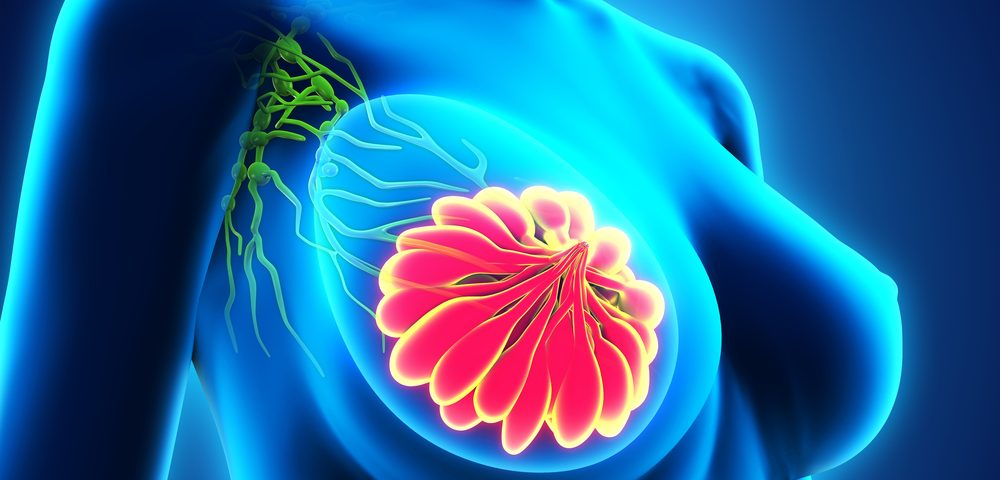
Women with breast cancer are at risk of having their disease spread to the lymph nodes, and from there elsewhere in the body. While lymph nodes in the axilla (armpit) are the most commonly affected, and are usually treated with surgery or radiation, the cancer may spread into lymph nodes behind the breast bone — called internal mammary (IM) lymph nodes – and then to those above the collar bone – called medial supraclavicular (MS) lymph nodes.
While IM-MS nodes can be treated with radiation therapy, concerns about the side effects of increasing the radiation area to the chest has limited such use.
In an attempt to settle this question, investigators designed a clinical trial that assessed the long-term outcomes in women receiving radiation to their IM-MS lymph nodes compared to a control group that did not.
The trial (NCT00002851), carried out by the European Organisation for the Research and Treatment of Cancer (EORTC), involved 4,004 women at 43 centers diagnosed with stage 1 through 3 breast cancer, who had undergone surgery to remove their breast tumor and nearby (axillary) lymph nodes.
Patients were divided in two groups: those who received 25 irradiation sessions over five weeks, and those who did not undergo further treatment.
After a median follow-up of 15.7 years, 1,117 patients had died. But researchers found that fewer patients in the radiation group had died from breast cancer compared to the control group — 15.8% vs. 19.7%. Similarly, the chance of cancer re-appearance was lower in patients who had received radiation treatment – 24.5% vs. 27.1%.
Overall survival was also higher in the group given this radiation treatment (73.2%) compared to control patients (70.8%).
“Our results make it clear that irradiating these lymph nodes gives a better patient outcome than giving radiation therapy to the breast/thoracic wall alone. Not only have we shown that such treatment has a beneficial effect on disease control, but it also improves breast-cancer related survival,” Philip Poortmans, head of the department of radiation oncology at the Institut Curie in Paris, said in a press release.
This 15-year follow-up is the second of three scheduled analyses planned for this Phase 3 clinical trial, with the last evaluation set for 20 years post-treatment. “We want to look further at which patients are most likely to benefit from this treatment, and to identify the best techniques for doing it efficiently and safely,” Poortmans said.
According to the researchers, side effects of IM-MS radiation treatment were largely minor and temporary, and included “no evidence … in the incidence of second malignancies, contralateral breast cancer, or cardiovascular deaths.”
“It is very important that we record all possible events, including recurrence and toxicity, and an even longer follow-up will also give us the opportunity to continue evaluating our patients in other areas, for example quality of life and wellbeing,” Poortmans said.
“Advances in radiation therapy techniques and new therapies, and earlier diagnosis may increase the benefit from IM-MS radiation treatment,” he concluded. “But we believe that our trial has already given solid evidence of the benefits of radiation treatment of the IM-MS lymph nodes.”