An international team of researchers has developed a wireless device that can detect early problems after a patient undergoes breast reconstruction surgery.
The work, led by Imperial College London in the U.K., and funded by the Engineering and Physical Sciences Research Council (EPSRC), was part of the Smart Sensing for Surgery project.
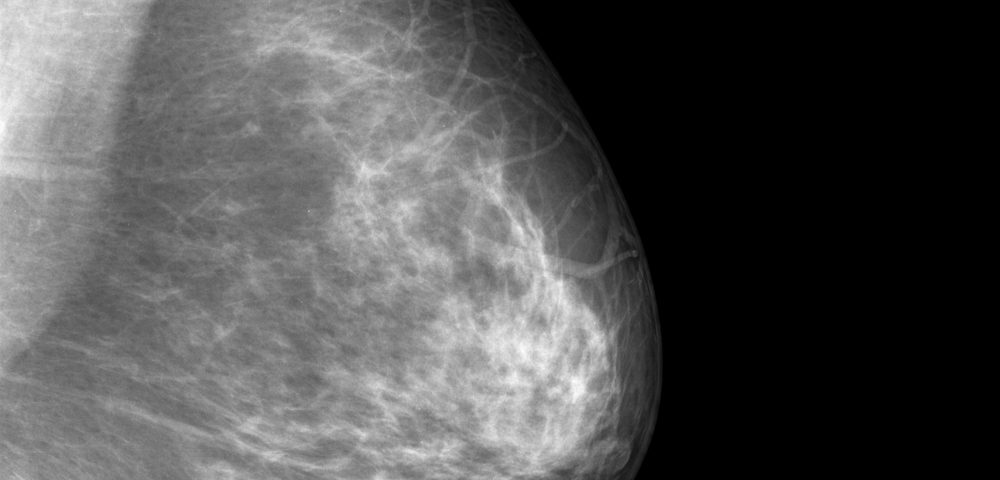
Breast reconstruction surgery following a mastectomy generally involves the transfer of the patient’s own tissue to help rebuild the breast. While the success rate of this procedure is high, early detection of potential problems could help to reduce post-surgical complications and prevent surgery failure.
“Poor blood supply or failure of breast reconstruction surgery can have a major impact on a breast cancer patient’s recovery, prognosis and mental wellbeing,” Guang-Zhong Yang, PhD, the lead researcher of the Smart Sensing for Surgery project, said in a press release. “Clinical signs of failure often occur late and patients may be returned to the operating room on clinical suspicion.”
To solve these problems, researchers have developed a wireless electronic device, a 1.8-by-1.1-cm bio-patch made of sensors encased in fully biocompatible materials, to monitor the levels of oxygen saturation in the transferred tissue, which is a reliable indicator of whether there is a risk of reconstruction failure.
Oxygen saturation levels are measured through a noninvasive imaging technique called near-infrared spectroscopy (NIRS), and the device captures and transmits encrypted data to maintain security and privacy.
In early clinical trials, the bio-patch was attached to a group of breast cancer patients for 48 hours following breast reconstitution surgery and was found to successfully and continuously monitor the levels of oxygen saturation in the tissues.
Yang noted their new device provides “objective data as an early warning system for medical staff, enabling earlier and simpler interventions, as well as giving patients increased peace of mind.”
The research team is working on securing funding to move to more advanced clinical stages, with the goal of making the bio-patch available for widespread clinical use within two to three years.
The new device is also being adapted to and tested to monitor other conditions, including dementia and chronic obstructive pulmonary disease (COPD).
The Smart Sensing for Surgery received just more than £3 million ($3.9 million) in EPSRC support and led to the development of other clinically helpful devices, such as “smart” catheters or drains that can detect infection-related problems early in time, and sensors of pulse rate, temperature, and pH balance that can be implanted under the skin.