Scientists have created a new artificial intelligence (AI)-based model that outperforms current models at predicting the risks a woman has of developing breast cancer, and works equally well in white and African American women.
The findings of the study, “A Deep Learning Mammography-based Model for Improved Breast Cancer Risk Prediction,” were published in Radiology.
Over the years, researchers attempted to create models incorporating information from genetic and hormonal factors that could estimate the risks a woman has of developing breast cancer. Unfortunately, most of these models failed to accurately predict the chances a patient has of developing the disease.
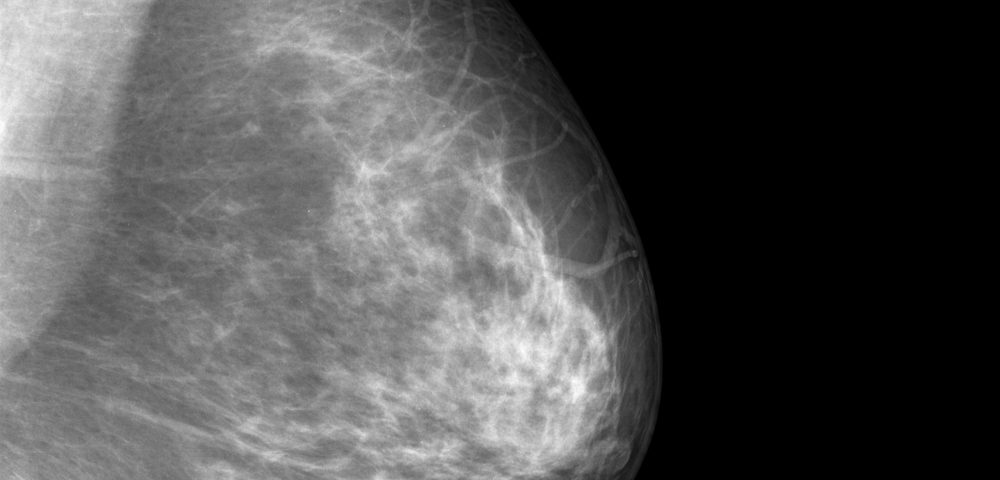
Mammographic breast density — the ratio between dense mammary tissue and fatty tissue in a woman’s breast assessed during a mammogram — is one of the independent risk factors for breast cancer that has received the most attention. For this reason, it has been added to multiple models to improve their accuracy at predicting breast cancer risk.
“The use of breast density as a proxy for the detailed information embedded on the mammogram is limited because breast density assessment is a subjective assessment and varies widely across radiologists. … [Essentially this means that] same-age patients who are assigned the same density score can have drastically different mammography with vastly different outcomes,” the researchers explained.
For this reason, developing an AI deep-learning model that would be able to pick up subtle differences in mammograms and analyze them in an automated, reproducible, non-biased way, might open the door to implementing stronger breast cancer prediction models.
In this study, researchers from the Massachusetts Institute of Technology (MIT) in collaboration with physicians from Massachusetts General Hospital (MGH) set out to develop a new AI-based prediction model that would outperform currently existing models at estimating the likelihood a woman has of developing breast cancer.
To do so, they used almost 90,000 mammogram screenings from approximately 40,000 women who had been examined at a large tertiary academic medical center from 2009 to 2012 to train, validate, and test the prediction capabilities of the new AI deep-learning model based on mammogram data.
In addition, they also compared the prediction capabilities of the new AI-based risk model to those of two other models: one based on conventional risk factors that also included breast density information (Tyrer-Cuzick model); and another hybrid deep-learning AI model that combined information from standard risk factors with data from mammograms.
Results showed that both AI deep-learning models outperformed the prediction capabilities of the standard Tyrer-Cuzick model by a large margin.
In addition, the hybrid AI deep-learning model maintained its accuracy among women from different age groups, ethnicities, and family histories.
“Unlike traditional models, our deep learning model performs equally well across diverse races, ages and family histories,” Regina Barzilay, PhD, said in a press release. Barzilay is an AI expert, professor at MIT, and corresponding author of the study.
“Until now, African-American women were at a distinct disadvantage in having accurate risk assessment of future breast cancer. Our AI model has changed that,” she said.
Despite the hybrid AI-based model being considered the best prediction model overall, the AI-model based only on information from mammogram screenings also had strong prediction capabilities, especially in the cases for which information from conventional risk factors was unavailable.
“This can be especially beneficial to patients who do not know their family history of breast or ovarian cancer. In addition, image-only DL [deep-learning] risk assessment could be rapidly implemented into breast imaging screening programs, with patient risk automatically assessed from the mammogram alone,” the investigators wrote.
The new AI deep-learning models already are being used for standard mammography screenings at MGH. Their performance is still being monitored, while researchers are working on developing new ways to convey this important breast cancer risk information to patients and their physicians.
“A missing element to support more effective, more personalized screening programs has been risk assessment tools that are easy to implement and that work across the full diversity of women whom we serve,” said Constance Lehman, MD, PhD, chief of breast imaging at MGH, professor of radiology at Harvard Medical School, and co-author of the study.
“We are thrilled with our results and eager to work closely with our health care systems, our providers and, most importantly, our patients to incorporate this discovery into improved outcomes for all women,” she said.