Trilaciclib, a treatment that protects the bone marrow from the damaging effects of chemotherapy, significantly extends the lives of women with metastatic triple-negative breast cancer receiving a chemotherapy regimen of gemcitabine and carboplatin, G1 Therapeutics announced.
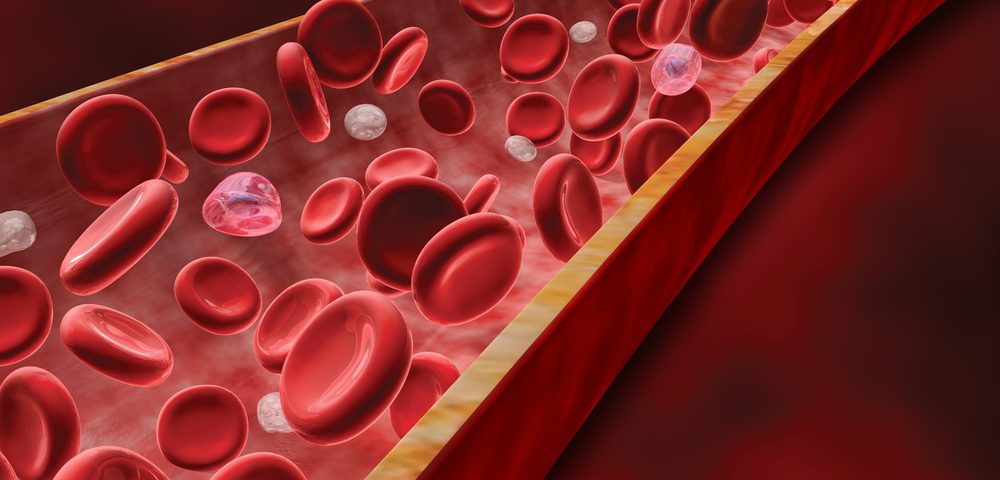
Chemotherapy kills tumor cells that divide rapidly. However, a major side effect is that it also kills rapidly-dividing healthy cells, including important stem cells in the bone marrow. Those stem cells produce white blood cells, red blood cells, and platelets.
Therefore, most chemotherapy agents cause bone marrow toxicity as a secondary effect. That leads patients to reduce their chemotherapy dose, or stop the treatment, which increases the chances of cancer progression.
Trilaciclib, developed by G1 Therapeutics, is a myelopreservation agent — meaning it protects the bone marrow from damage caused by chemotherapy. Combining chemotherapy and myelopreservation agents increases the amount of chemotherapy that individuals can tolerate, thus improving patient outcomes.
The treatment’s protective effects were demonstrated in lung cancer patients, but their need for supportive care and dose reductions is significantly lower. Now, trilaciclib is being evaluated in metastatic triple-negative breast cancer patients — a population whose chemotherapy treatment is often limited by bone marrow toxicity.
An ongoing, randomized, Phase 2 clinical trial (NCT02978716) is comparing the effects of a combination of trilaciclib and chemotherapeutic agents gemcitabine and carboplatin, with that of chemotherapy alone. The trial involves 102 participants who had received up to two prior lines of therapy.
Participants were divided into three groups: chemotherapy alone, chemotherapy and trilaciclib the day of chemotherapy, and chemotherapy and trilaciclib the day before and the day of chemo.
The first findings from the trial were presented at the 2018 San Antonio Breast Cancer Symposium. They showed that adding trilaciclib to chemotherapy significantly reduced the occurrence of major blood-related adverse events, meaning that bone marrow toxicity was reduced. The treatment also increased the amount of chemotherapy participants tolerated.
Response rates and progression-free survival — the time patients lived without disease worsening — were better among those receiving trilaciclib. These patients lived a median of 7.9 months without disease progression, compared with 5.4 months for those on chemo only. Overall, trilaciclib was well-tolerated, and the combination showed an adverse event profile similar to chemotherapy alone. There were no adverse events related to trilaciclib.
Now, G1 revealed additional data from the trial, showing that both doses of trilaciclib significantly increased the overall survival of participants, compared with chemotherapy alone.
“Triple-negative breast cancer (TNBC) is the most aggressive type of breast cancer, and women diagnosed with metastatic TNBC need new treatment options. We look forward to sharing these data with regulators, as well as presenting findings from this trial at a medical meeting later this year,” Mark Velleca, MD, PhD, G1 Therapeutics’ CEO, said in a press release.
G1 also is expecting to initiate other randomized trials to evaluate trilaciclib’s capacity to protect the bone marrow in different tumor types, and combined with other chemotherapy agents.