Breast cancer cells with mutations in the BRCA1 or BRCA2 genes can become resistant to chemotherapy drugs by recruiting a host of proteins that protect tumor DNA from damage.
Since mutations in the BRCA1 and BRCA2 genes cause flaws in DNA repair processes, increasing the risk of breast, ovarian, and other types of cancer, the study “Replication fork stability confers chemoresistance in BRCA-deficient cells,” published in the journal Nature, demonstrates how a tumor balances the need for new mutations with the ability to protect itself from extensive DNA damage.
In the short term, the findings might allow physicians to predict the response to DNA-damaging chemotherapy by measuring the levels of these proteins. In a longer perspective, they may also help cancer scientists find ways around tumor resistance to chemotherapy, a serious problem in cancer treatment.
The BRCA1 and BRCA2 genes code for proteins that continuously survey DNA, looking for and repairing damage. Mutations in these genes disrupt the process and are found in up to 10 percent of all breast cancer patients. While the mutations are the culprit causing cancer in the first place, the inability of BRCA1 and 2 to mend broken DNA also makes tumor cells particularly sensitive to DNA-damaging cancer treatment. Over time, however, many tumors become resistant to such drugs.
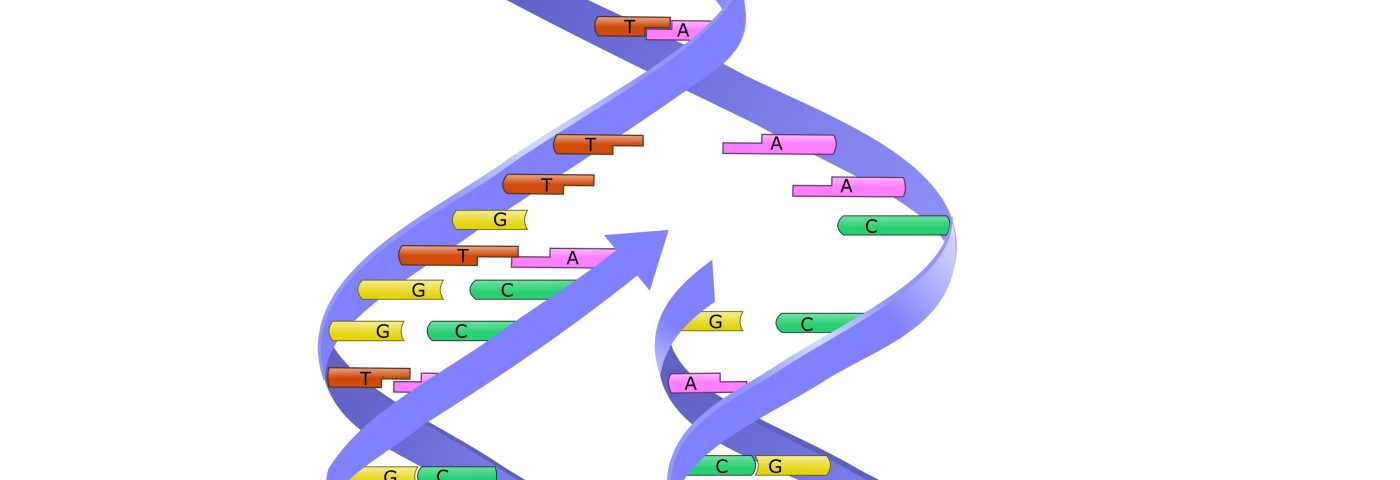
Andre Nussenzweig, PhD, and his research team at the National Cancer Institute have been studying DNA repair processes for the past decade, and are focusing on the protection of DNA during replication, or DNA-copying. The process occurs at specific spots along the DNA strand called replication forks. As the fork moves along a DNA strand, it can be stopped by a group of factors called replication fork barriers. When the fork stops moving, the BRCA1 and BRCA2 proteins quickly arrive to protect the newly synthesized DNA by repairing double strand breaks. If this process is absent, as is the case in BRCA1/2 tumors, the DNA is soon degraded, making cells sensitive to drugs blocking the DNA copying processes.
But the research team found that tumors can get around this problem. Instead of fixing the repair, tumors were seen to employ another set of factors involved in the breakdown of the newly synthesized DNA. When these factors were missing, the DNA-degrading enzyme was prevented from doing its work at the fork — a strategy cancer cells use to protect themselves from drugs. The finding has clinical implications for cancer treatment, as studies have shown that the levels of these factors predict how well patients with BRCA1 or 2 mutations respond to chemotherapy.
Researchers also showed that removing different factors in this group led to the same protection against DNA degradation, showing that tumors use complex strategies to evade treatment.
“It is the intricate mechanisms that tumor cells evolve to bypass the need for accurate DNA repair that form the foundation of our study,” Nussenzweig said in a news release. “A deeper knowledge of the processes that drive drug resistance in BRCA1/2-mutant tumors will lead to novel therapeutic approaches that target tumor-specific vulnerabilities.”