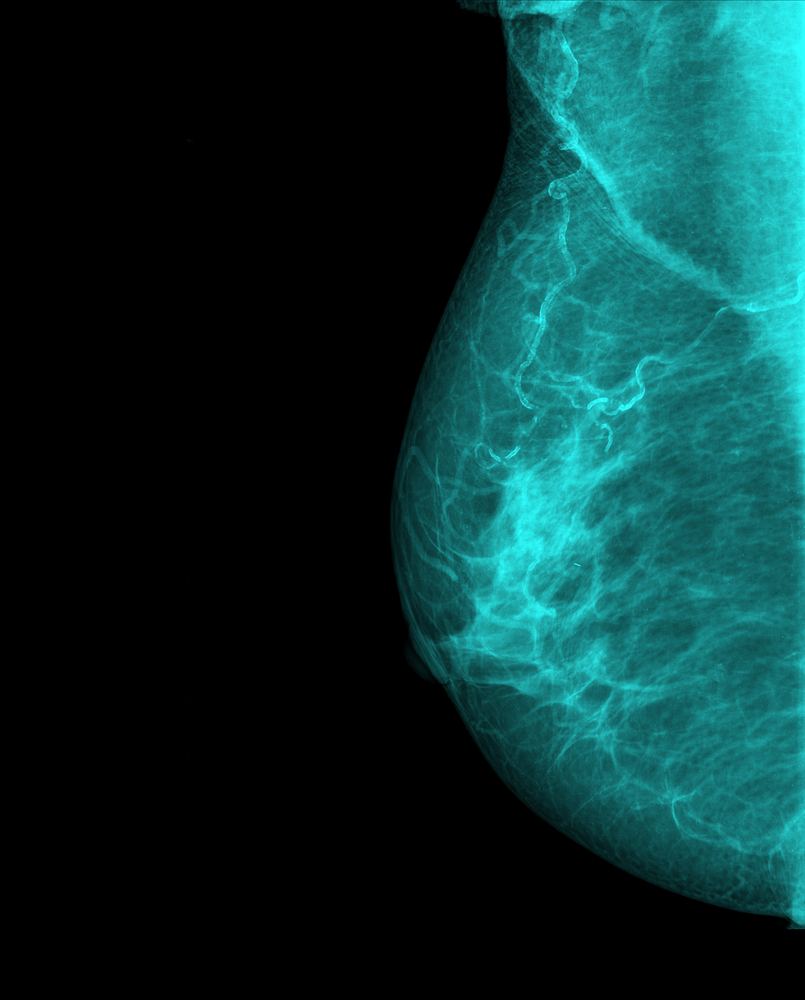
 The perfect recipe for metastatic breast cancer uses an endothelial cell, a perivascular macrophage, and a tumor cell that produces high levels of a protein called Mena, according to new work from Albert Einstein Cancer Center and Montefiore Einstein Center for Cancer Care.
The perfect recipe for metastatic breast cancer uses an endothelial cell, a perivascular macrophage, and a tumor cell that produces high levels of a protein called Mena, according to new work from Albert Einstein Cancer Center and Montefiore Einstein Center for Cancer Care.
Maja Oktay, MD, PhD, in the department of pathology, led a study that investigated this combination of cells using patient-derived breast cancer tumor cells and in vitro-cultured blood vessel lining cells (endothelial cells).
As motivation for this work, Dr. Oktay stated in a news release, “The outcome for patients with metastatic breast cancer hasn’t improved in the past 30 years despite the development of targeted therapies. It’s critically important to learn more about the metastatic process so we can develop new ways to predict whether cancer will spread and identify new treatments”.
To begin the learning process, Dr. Oktay’s laboratory first looked to earlier studies that combined animal models and human cancer cell lines. A number of studies identified that the trio of cells provides a location at which tumor cells enter blood vessels–it is known as the tumor microenvironment of metastasis (TMEM). Based on the number of these locations, a TMEM score can be applied to patients’ tumors and indicate the likelihood for metastasis.
In addition to a high TMEM score, high levels of Mena in the MenaINV form put patients more at risk for metastatic tumors. “Those studies revealed new insights into how cancer might spread, but they didn’t necessarily show what is happening in those patients,” said Dr. Oktay.
She addressed this gap in the paper “Invasive Breast Carcinoma Cells from Patients Exhibit MenaINV– and Macrophage-dependent Transendothelial Migration,” which was published in Science Signaling. The team characterized cancer cell penetration of the inner layer of blood vessels by extracting tumor cells from patients, placing them on single layers of endothelium, and monitoring their migration across the barrier. Cells that expressed high levels of MenaINV crossed the endothelium more readily.
[adrotate group=”3″]
In another experiment, the researchers analyzed tissue biopsies from tumors from 60 breast cancer patients and assigned a TMEM score. High TMEM score correlated with high levels of MenaINV. “These results confirm that TMEM sites and MenaINV are essential for the spread of breast cancer in humans,” said Dr. Oktay. “They also imply that MenaINV expression and TMEM score measure related aspects of a commonly used mechanism that human breast cancers use to metastasize.”
At the moment, Dr. Oktay’s team is collaborating with MetaStat, Inc. to develop and commercialize a TMEM test to determine a patient’s risk for metastatic breast cancer. Perhaps this test can be used to alert patients and clinicians to the need for more aggressive treatment to increase the chances of survival for breast cancer patients.