Researchers from the University of Rochester Medical Center (URMC) in Rochester, NY recently released the results of a study that provides evidence of a treatment strategy that could increase the effectiveness of a chemotherapeutic agent’s ability to kill cancer cells. The study entitled, “Attenuation of nonsense-mediated mRNA decay facilitates the response to chemotherapeutics,” was published in the latest edition of Nature Communications.
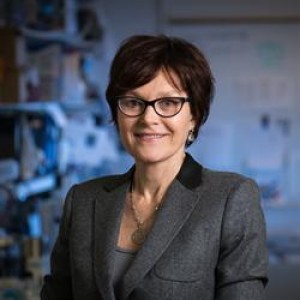
The study was conducted in the laboratory of Dr. Lynne E. Marquat, PhD, J. Lowell Orbison Endowed Chair and Professor in the Department of Biochemistry and Biophysics, Director of the Center for RNA Biology, Founder of the University of Rochester Graduate Women in Science Program, URMC. For over 30 years, Dr. Marquat has conducted research into discovering new cellular pathways and clues to the molecular basis of human disease, with a recent focus on understanding the quality control mechanisms of nonsense-mediated mRNA decay (NMD). For this and many other contributions she has made to the field of RNA science, Dr. Marquat was elected to the National Academy of Sciences, and was also a recipient of the 2015 Gairdner International Award, Canada’s major international science prize for medical researchers whose work contributes significantly to improving the quality of human life.
The importance of Dr. Maquat’s work is described by her colleague and fellow innovative cancer researcher Dr. Hartmut Land, PhD, Chair of the Department of Biomedical Genetics and Scientific Director of the Wilmot Cancer Center, URMC, “The work from Lynne Maquat’s lab is critical because it demonstrates the role for NMD in cancer cell survival and shows us how the NDM pathway might be connected to chemotherapy response.”
Study Methods
In this study, Dr. Marguett and her post-doctoral fellow Dr. Maximilian Popp, PhD, who was the only co-author on the paper, conducted the following laboratory experiments to assess the relationship between NMD and the effectiveness of doxorubicin, a chemotherapy agent used most often to treat patients with breast cancer (BC):
- They first exposed BC cells with doxorubicin alone and measured the number of cells that were still alive after treatment.
- Secondly, they exposed BC cells with doxorubicin and a compound that inhibits NMD and measured the number of cells that were still alive after treatment.
- Finally, they exposed BC cells with the compound that inhibits NMD, removed the compound after several hours, and then treated cells with doxorubicin. Afterwards they measured the number of cells that were still alive after treatment.
In a URMC press release, Dr. Popp described NMD as “the body’s way of proof reading messenger RNA or mRNA, which takes genetic instructions from DNA and uses it to create proteins that carry out our body’s functions. NMD flags and derails the production of unwanted proteins that can disrupt normal processes and initiate disease, like an inspector flags and removes faulty products from an assembly line.”
[adrotate group=”3″]
Study Results
The results of the experiments showed that the final test in which the NMD-inhibiting compound was used followed by doxorubicin was the most effective at killing cancer cells: the BC cells were 2.5 times more likely to die using that method versus exposing BC cells to doxorubicin alone. The reasoning behind this observation is not completely understood by the team but they surmise that inhibiting the quality-control mechanisms of NMD allows an increase in apoptosis (cell death) during exposure to the chemotherapeutic agent.
They did stress that inhibiting NMD alone was not enough to effectively kill BC bells, but that doxorubicin was also necessary to make a therapeutic impact. When discussing the results, Dr. Popp stated, “The idea of combining a drug that inhibits NMD with chemotherapy that is already used to treat a wide range of cancers has the potential to impact patient care. We don’t completely understand the detailed mechanisms by which NMD operates, so there is still a lot of work to do, but this study gives us a path forward.”
For Dr. Maquat, “This research highlights the importance of basic research and its relevance to human disease and therapies.”
This work is in its early stages and there needs to be confirmatory studies conducted in the lab to eventually conduct human clinical trials, but Drs. Maquat and Popp believe their data provide insights that could lead to new treatment strategies for cancer patients in the future.
Dr. Maquat hopes that the success of her laboratory work will inspire young people especially girls and young women to think about a career in science.