A measure signed into law by Oklahoma Gov. Mary Fallin on April 21 will require healthcare providers to notify women who may be at an increased risk of breast cancer. Under House Bill 2601, sponsored by state Rep. Mike Ritze, healthcare facilities are obliged to include breast density information in all mammography reports, and to additionally notify patients with extremely dense breast tissue that they may be at increased risk of developing breast cancer.
A measure signed into law by Oklahoma Gov. Mary Fallin on April 21 will require healthcare providers to notify women who may be at an increased risk of breast cancer. Under House Bill 2601, sponsored by state Rep. Mike Ritze, healthcare facilities are obliged to include breast density information in all mammography reports, and to additionally notify patients with extremely dense breast tissue that they may be at increased risk of developing breast cancer.
 “Dense breast tissue is not abnormal,” said Rep. Ritze, a board-certified physician, in a release, “but it does make it more difficult to detect abnormalities and leads to an increased risk of cancer.”
“Dense breast tissue is not abnormal,” said Rep. Ritze, a board-certified physician, in a release, “but it does make it more difficult to detect abnormalities and leads to an increased risk of cancer.”
“This is an effort to ensure that women have the information they need to make informed decisions about their health,” added Rep. Ritze (R-Broken Arrow), who is chair of the Oklahoma House Public Health Committee. “When patients are empowered with information, they are far more likely to act upon that information and take steps to reduce their risk.”
He emphasized that the measure, which comes into effect in November, does not create a duty of care or other legal obligation beyond the duty to provide notice. The bill also clarifies that any notice inconsistent with the federal Mammography Quality Standards Act is not required.
Oklahoma is now the 26th state to require dense breast tissue reports for patients, and several other states are expected to follow suit. A federal density reporting bill in both the House and Senate was also introduced in 2015. Currently, states protecting their citizens from missed, delayed, and advanced cancers because of dense breast tissue are: Connecticut (2009); Texas (2011); Virginia, New York, and California (2012); Tennessee, Hawaii, Maryland, Alabama, Nevada, Oregon, North Carolina, and Pennsylvania (2013); Ohio, Missouri, Massachusetts, Rhode Island, Minnesota, Arizona, and New Jersey (2014); Louisiana, Delaware, North Dakota, and Michigan (2015); Indiana and Oklahoma (2016).
 Connecticut became the first state to disclose density to patients in 2009, inspired by patient-turned-advocate Nancy M. Cappello, PhD. Dr. Cappello’s own cancer was masked on mammography by her dense breast tissue for years, in spite of her getting yearly mammograms. Her cancer was not diagnosed until it was at an advanced stage 3C, with 13 metastasized lymph nodes. Dr. Cappello’s advocacy led to establishment of two global nonprofit organizations: Are You Dense, Inc., and Are You Dense Advocacy, Inc., a 501(c)(4) tax exempt organization.
Connecticut became the first state to disclose density to patients in 2009, inspired by patient-turned-advocate Nancy M. Cappello, PhD. Dr. Cappello’s own cancer was masked on mammography by her dense breast tissue for years, in spite of her getting yearly mammograms. Her cancer was not diagnosed until it was at an advanced stage 3C, with 13 metastasized lymph nodes. Dr. Cappello’s advocacy led to establishment of two global nonprofit organizations: Are You Dense, Inc., and Are You Dense Advocacy, Inc., a 501(c)(4) tax exempt organization.
“I am honored to work with Representative Mike Ritze on behalf of Oklahoma women. Dr. Ritze understands the impact of dense breast tissue on missed, delayed and advanced stage breast cancers. His advocacy to report density to patients, through the mammography report, enhances breast screening and breast health discussions between patients and their health care providers,” Dr. Cappello said in a release.
With an estimated 40 percent of women having dense breast tissue that may mask the presence of cancerous tissue in standard mammography — which is about 48 percent effective in detecting lesions in dense breasts — women with dense breast tissue need to be informed of their status. Goals of groups like Are You Dense are advocacy of and support for state and federal legislative and regulatory efforts to standardize the communication
be informed of their status. Goals of groups like Are You Dense are advocacy of and support for state and federal legislative and regulatory efforts to standardize the communication
of dense breast tissue information to women.
In the research letter, “Content, Readability, and Understandability of Dense Breast Notifications by State” (JAMA. 2016;315(16):1786-1788. doi:10.1001/jama.2016.1712), published April 26 by the Journal of the American Medical Association (JAMA), co-author Nancy R. Kressin, PhD, of the Veterans’ Affairs Boston Healthcare System at Boston University School of Medicine, and colleagues reported a study evaluating the content and reading level of text in state-mandated dense breast notifications sent to women, noting that some of these notifications include terminology that is too technical for a patient audience, with the content of letters varying from state to state, and failing to clearly define next steps for patients who might benefit from additional screening.
The investigators noted that because dense breasts can mask cancer on mammography (masking bias), and are an independent cancer risk factor, evidence does not yet indicate whether or what supplemental screening is appropriate. Rather, the study’s investigators propose risk stratification to determine who may benefit from supplemental screening (eg: magnetic resonance imaging for women at high risk).
“Now that 26 states have adopted breast density notification laws, our ability to measure density and communicate the results to patients is more important than ever. An estimated 40% of women have dense breast tissue that may mask the presence of cancerous tissue in standard mammography. As breast density increases, mammography sensitivity decreases. As a radiologist, I have seen first-hand how dense breast tissue can make it more difficult to identify cancer in mammography,” Rachel Brem, MD, a board certified radiologist, vice chair of radiology, and director of Breast Imaging and Intervention Center at George Washington University, exclusively told Breast Cancer News.
She highlights how important it is for the medical community to ensure women fully understand their breast density, and whether they might benefit from additional screening, encouraging dialogue that can help patients to learn more about their individual risks and make informed decisions about their treatment.
“The study highlights how important it is for the medical community to ensure patients fully understand what their breast density is, and whether they might benefit from additional screening,” Dr. Brem added. “These communications are not meant to replace conversations with physicians; they should instead encourage a dialogue that can help patients learn more about their individual risks so they can make informed decisions about their treatment.”
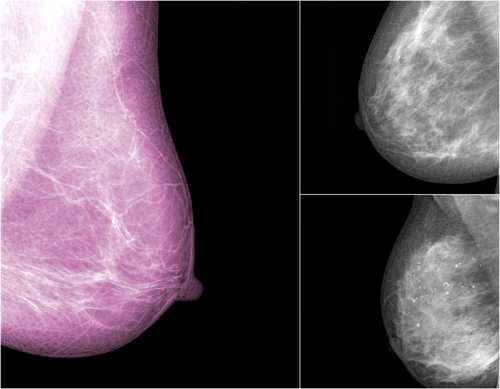
 There is also a new technology, iReveal by the Nashua, New Hampshire-based medical technology firm iCAD, designed for radiologists reading mammography who want to standardize assessment and reporting of breast density. iReveal helps clinicians identify patients whose dense breast tissue may impact the ability of mammography to clearly identify potentially dangerous lesions, and those who may benefit from supplemental screening or surveillance protocols.
There is also a new technology, iReveal by the Nashua, New Hampshire-based medical technology firm iCAD, designed for radiologists reading mammography who want to standardize assessment and reporting of breast density. iReveal helps clinicians identify patients whose dense breast tissue may impact the ability of mammography to clearly identify potentially dangerous lesions, and those who may benefit from supplemental screening or surveillance protocols.
iReveal uses an “appearance-based” approach to assess breast structure, texture, and fibroglandular dispersion to simulate the process radiologists use to measure breast density, and provide automated, rapid, and reproducible breast density results.
“It should be noted, the way breast density is assessed is just as important as the manner in which we communicate results to patients. A new technology, the iCAD iReveal automated breast density solution, now makes it possible to produce automated, rapid and reproducible assessments of breast density to more precisely identify patients who could benefit from additional screening,” Dr. Brem said. “Without technology that can accurately and consistently assess breast density, radiologists reading mammography might vary in their assessment of patients’ breast density, which could result in inaccurate readings and delays in getting patients the additional testing and possible treatment they need.”
For more information, visit: www.icadmed.com/ireveal.html#sthash.FDdKTqUE.dpuf
Sources:
Are You Dense Advocacy, Inc.
Government of Oklahoma
Journal of the American Medical Association (JAMA)
iCAD