Tumor blood vessels are chaotic with poor and restricted blood flow compared to vessels in healthy tissues, a problem that limits cancer treatments from reaching tumors via the bloodstream. But researchers have developed an antibody, called ABTAA, that might be used to re-establish the structural and functional integrity of the tumor vasculature.
The study, “Normalization of Tumor Vessels by Tie2 Activation and Ang2 Inhibition Enhances Drug Delivery and Produces a Favorable Tumor Microenvironment,” published in Cancer Cell, shows that ABTAA may not only reduce tumor aggressiveness, but also improve delivery of anti-cancer drugs to tumor sites.
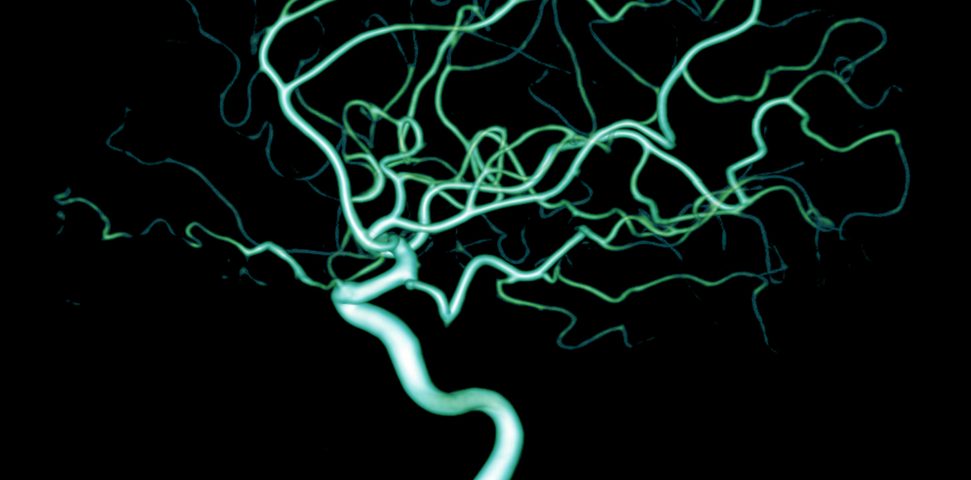
In healthy tissues, blood vessels form a patterned and functioning vasculature with a hierarchical organization of arteries, capillaries, and veins. Such vessels are lined by closely attached endothelial cells, and surrounded by pericytes that help to maintain their integrity and support blood flow without collapsing.
In established tumors, the vasculature is highly dysfunctional and lacks hierarchical organization. These vessels also lack an intact vessel wall, showing broken endothelial junctions and pericytes that are often detached. As a result, blood flow within the tumor is severely restricted, and the tumor becomes hypoxic — registering low oxygen levels.
This is important because tumors are known to transform in response to hypoxia, altering their microenvironment and becoming more aggressive and metastatic.
“When the tumor is established, hypoxia is the main driver of tumor progression. So, if we eliminate hypoxia, we make the tumor more mild, by reducing its progression and metastasis,” Gou Young Koh, director of the Center for Vascular Research, said in a press release.
The researchers came up with a way to change the tumor vasculature, marking it more “normal,” by exploring a signaling pathway that is involved in blood vessel formation and integrity, the Ang2/Tie2 pathway.
“Tumor can adapt to hypoxia and get more aggressive, so we tried to prevent this transition by normalizing tumor vessels,” said Jin-Sung Park, the study’s first author. “We call it normalization of tumor vessels, because it resembles closely the wall architecture of healthy, normal vessels.”
ABTAA, which stands for Ang2-Binding and Tie2-Activating Antibody, is an unsual antibody that simultaneously inhibits Ang2 and activates Tie2. This reduces vessel instability and induces the pericytes to reattach to the vessel wall.
“ABTAA changes the whole tumor environment, oxygenation status and level of lactate, so that the immune cells and drugs can reach the core regions of the tumor more easily. In this way, we create a favorable ground for tumor treatment,” Park said.
The researchers tested ABTAA in mice with three different tumor types — glioma (brain tumor), and lung and breast cancer — both alone and in combination with other anti-cancer drugs. They found that ABTAA alone was sufficient to reduce tumor size. But when combined with chemotherapies, the effects were more striking.
Indeed, while the chemotherapeutic drug temozolomide reduced tumor growth by 36 percent in the glioma mice model, temozolomide administered in combination with ABTAA decreased growth by 76 percent.
Similarly, ABTAA combined with Platinol (cisplatin) in a breast cancer mouse model reduced tumor growth more effectively than either Platinol or ABTAA alone.
“[O]ur findings establish that simultaneous Tie2 activation and Ang2 inhibition form a powerful therapeutic strategy to elicit a favorable tumor microenvironment and enhanced delivery of a chemotherapeutic agent into tumors,” the team concluded.