A newly developed online prognostic tool can determine whether a woman is at high risk of cancer recurrence or spread after receiving the standard five years of hormone therapy, and whether she could benefit from extended treatment, a study shows.
The tool, called CTS5, is made for women with estrogen receptor-positive breast cancer and was developed by researchers at The Royal Marsden NHS Foundation Trust and Queen Mary University of London.
“What we have developed could improve clinical practice, benefiting breast cancer patients by avoiding potentially unnecessary extended treatment,” Mitch Dowsett, head of The Royal Marsden Ralph Lauren Centre for Breast Cancer Research, professor at The Institute of Cancer Research, London, and study first author, said in a press release.
“Clinicians require expertise and the best tools to help them make crucial decisions on treatment for patients, decisions that can make a difference to patients’ quality of life,” he added.
The study, “Integration of Clinical Variables for the Prediction of Late Distant Recurrence in Patients With Estrogen Receptor-Positive Breast Cancer Treated With 5 Years of Endocrine Therapy: CTS5,” was published in the Journal of Clinical Oncology.
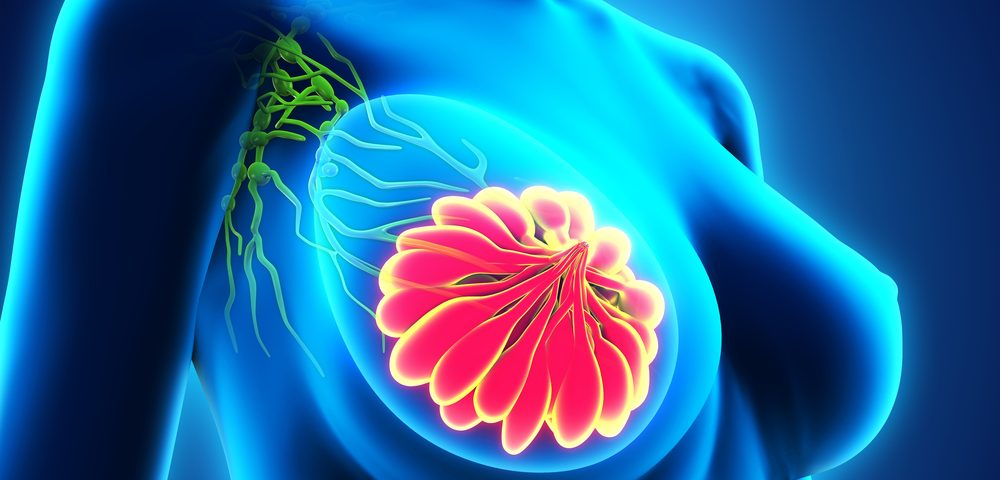
Estrogen receptor (ER)-positive breast cancer accounts for about 85 percent of all breast cancer cases in the Western world. Patients are usually treated with surgery, chemotherapy and/or radiation, followed by hormone therapy for five years to lower their risk of cancer recurrence and spread.
In more than half of the cases, however, cancer metastasis occurs after this five-year period. Extending hormone therapy reduces the rate of cancer recurrence, but the effects are modest and some patients may experience adverse side effects, including bone weakness and menopausal symptoms. Thus, identifying patients whose risk of cancer metastasis is low would prevent them from receiving a treatment that would bring little benefit and potential adverse effects.
Aiming to do that, researchers developed a simple prognostic tool to estimate risk of cancer metastasis after five years of hormone treatment. They called it Clinical Treatment Score post-5 years or CTS5.
The tool was developed using data from the ATAC trial (ISRCTN18233230), a study where 4,735 postmenopausal women with ER-positive or ER-unknown early breast cancer received hormone therapy — Arimidex (anastrozole), tamoxifen, or a combination — for five years.
Women were followed for a median of 9.8 years and researchers assessed how many developed cancer metastasis within five to 10 years of finishing hormone therapy. This information was combined with tumor characteristics to create the CTS5 test.
To test the tool, researchers then examined data from another trial, called BIG 1-98 (NCT00004205). In this trial, 6,711 postmenopausal women with hormone receptor-positive early stage breast cancer received five years of daily treatment with Femara (letrozole) or tamoxifen.
The trial also tested a sequential therapy, with patients receiving two years of Femara followed by three years of tamoxifen, or the other way around. Women were followed for a median of 8.1 years.
After inserting patient details, including age, tumor size, and tumor grade, CTS5 was able to stratify women according to their risk for cancer metastasis: low risk meant that their changes of cancer recurrence in distant organs were below 5%, intermediate was linked to a risk between 5% and 10%, and women at high risk had more than a 10% chance of seeing their cancer spreading.
Overall, 42% of the women were categorized as low risk, meaning that extending their hormone therapy would probably not add any benefit and might even promote adverse effects.
The CTS5 is available to clinicians and is used as a calculator to predict a patient’s risk for cancer recurrence and metastatsis.
“Hormone-sensitive breast cancer is one of the few cancers where late recurrence is common, and predicting who is at high risk is particularly important so that they can continue hormone treatment. While our ability to predict this type of cancer is highly likely to improve in the future, we’re providing a simple tool which is available now, and is easily used and well-tested,” said Jack Cuzick, study senior author and professor at the Queen Mary University of London.
“Our tool provides a very simple way of obtaining the risk of a late metastasis for each woman individually. It is very important to identify these women in the clinic and the calculator provides help in the decision-making process,” said Ivana Sestak, also an author in the study.